Testosterone deficiency, also known as hypogonadism, is a state with sub-optimal circulating levels of testosterone concomitant with clinical signs and symptoms attributed to low physiological testosterone levels.[1-3]
Sexual dysfunction is the most commonly recognized symptom of testosterone deficiency. However, testosterone also plays a broader role in men’s health. A growing body of evidence has established associations between low testosterone levels and multiple risk factors and diseases including the metabolic syndrome, obesity, type 2 diabetes, sarcopenia, frailty, mobility limitations, osteoporosis, cognitive impairment, depression, cardiovascular disease, and reduced longevity.[3-12]
In this article I provide an overview of the detrimental impact of testosterone deficiency on a wide range of health outcomes.[13]
KEY POINTS
Adverse effects of testosterone deficiency (TD) on men’s health.[13]
What is known
Testosterone deficiency is characterized by either deficiency in total serum testosterone (TT) levels or low calculated free testosterone levels (below the young healthy adult male reference range), coupled with signs and symptoms indicative of sup-optimal testosterone levels. [1-3] While there is no universal agreement on the specific signs and symptoms of testosterone deficiency, reduced sexual desire and sexual dysfunction are thought to be strong indications of testosterone deficiency.[1-3, 14-18] More specifically, the three sexual symptoms most significantly related to low testosterone levels are decreased frequency of morning erection, decreased frequency of sexual thoughts, and erectile dysfunction.[18] Other signs and symptoms include reduced physical performance (an inability to engage in vigorous activity [e.g., running, lifting heavy objects, or participating in strenuous sports], an inability to walk more than 1 km, and an inability to bend, kneel, or stoop), and psychological malaise (loss of energy, sadness [“downheartedness” on questionnaire], and fatigue).[18]
Clinically, testosterone deficiency is divided into primary hypogonadism (testicular dysfunction), secondary hypogonadism (pituitary or hypothalamic failure) or mixed hypogonadism (a combination of testicular failure and pituitary-hypothalamic failure).[3] A significant proportion of older men have high gonadotropins (LH and FSH) and testosterone within the normal range.[19-21] This indicates a state of compensated, or subclinical, hypogonadism that may eventually develop into overt primary hypogonadism. [22] Thus, by coupling testosterone levels with LH levels clinicians can detect impending testosterone deficiency. Measuring LH together with testosterone can also strengthen symptomatic diagnosis as sexual symptoms are more prevalent in secondary and primary hypogonadism, whereas physical symptoms are more likely in compensated hypogonadism. [22] Obese men are especially prone to secondary hypogonadism, while in older men primary hypogonadism predominates. [22] Testosterone deficiency may also result from an impairment of testosterone action because of decreased bioavailability of the hormone (due to SHBG elevations) or because of androgen receptor alterations.[3]

It is important to note that low testosterone levels even within the normal range negatively impact risk of cardiovascular events and mortality. For example, the MrOS (Osteoporotic Fractures in Men) Study found that men aged 69 to 81 years in the highest quartile of testosterone, 550 ng/dL (approximately 19.1 nmol/L) and above, had a lower risk of cardiovascular events compared with age-matched men in the 3 lower quartiles.[23] More specifically, men having testosterone levels of 550 ng/dl and above had a 30% lower risk of experiencing cardiovascular events during a 5 year follow-up compared to men with levels below 550 ng/dL.[23] This association remained after adjustment for traditional CV risk factors and was not materially changed in analyses excluding men with known CV disease at baseline.
The EPIC-Norfolk (European Prospective Investigation Into Cancer in Norfolk) Prospective Population Study demonstrated in men aged 40 to 79 years that increasing endogenous testosterone levels are inversely related to mortality due to all causes, cardiovascular causes, and cancer during a 7 year follow-up. [24] Men in the highest (over 19.6 nmol/L = 565 ng/dL) compared with the lowest quartile (below 12.5 nmol/L = 361 ng/dL) of testosterone level had a 25-30% lower risk of total mortality.[24] The EPIC-Norfolk Study also found that for every 6-nmol/L (173 ng/dL) increase in serum testosterone there was a 14% lower risk of mortality. The magnitude of effect was similar for deaths due to cardiovascular causes and those due to cancer and was little changed after adjustment for cardiovascular risk factors and sex hormone binding globulin or after the exclusion of deaths within 2 years.[24] Also in men with pre-existing coronary artery disease low testosterone levels within the normal range negatively impact survival, with a cut-off of total testosterone of 15.1 nmol/L (436 ng/dL) being related to increased mortality.[25]
It should be underscored that all these thresholds represent cut-offs that are higher than most currently accepted definitions of hypogonadism. In many laboratories, the lower limit of the normal range for total testosterone levels is 280-300 ng/dl (9.8–10.4 nmol/L). [1] Thus, even men who have not been diagnosed with hypogonadim and therefore are being denied testosterone therapy may be at unnecessarily increased risk for negative health outcomes, which may be prevented with testosterone therapy.
What new research shows
Testosterone deficiency, which is a common clinical condition, is associated with many adverse health effects and a significant deterioration in quality of life, see key points table above.
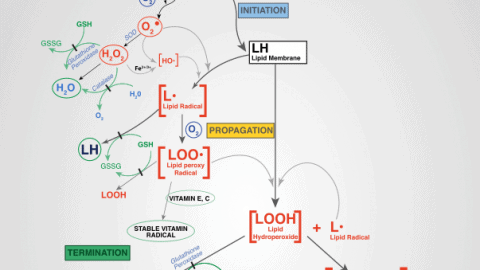
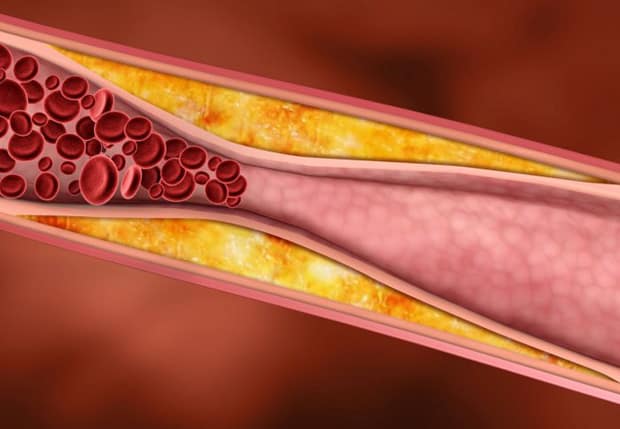
Testosterone deficiency increases risk for obesity, type 2 diabetes, metabolic syndrome, cardiovascular disease, dyslipidemia, inflammation, endothelial dysfunction, hypertension, and loss of lean body mass, muscle volume and strength, and bone mineral density. Testosterone deficiency is also associated with diminished sexual desire and erectile function, decline in cognitive and intellectual function, reduced energy, increased fatigue, depressed mood and vitality, and depression. Figure 1 below illustrates how testosterone deficiency contributes to development or progression of multiple risk factors, which in turn increase the risk of mortality.
Figure 1: Testosterone deficiency in men contributes to a host of co-morbidities. These include, inflammation, insulin resistance, diabetes, dyslipidemia, hypertension, metabolic syndrome, vascular stiffness, atherosclerosis, cardiovascular disease, sexual dysfunction and mortality.
Men with erectile or ejaculatory dysfunction, reduced sexual desire, as well as those with expanded bellies (visceral obesity) and metabolic diseases, should be screened for testosterone deficiency and if found hypogonadal, treated, regardless of age.[3, 14] Because testosterone therapy in testosterone deficient men with these co-morbidities may reverse or delay their progression [26], it is imperative that clinicians become more aware of the wide ranging impact of sub-optimal testosterone levels on men’s health and well-being.
In the next article I will go into detail on the wide range of health promoting effects of testosterone replacement therapy in men with hypogonadism. Stay tuned….
References:
1. Bhasin, S., et al., Testosterone therapy in men with androgen deficiency syndromes: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab, 2010. 95(6): p. 2536-59.
2. Wang, C., et al., Investigation, treatment, and monitoring of late-onset hypogonadism in males: ISA, ISSAM, EAU, EAA, and ASA recommendations. J Androl, 2009. 30(1): p. 1-9.
3. Buvat, J., et al., Testosterone deficiency in men: systematic review and standard operating procedures for diagnosis and treatment. J Sex Med, 2013. 10(1): p. 245-84.
4. Saad, F., Androgen therapy in men with testosterone deficiency: can testosterone reduce the risk of cardiovascular disease? Diabetes Metab Res Rev, 2012. 28 Suppl 2: p. 52-9.
5. Saad, F. and L. Gooren, The role of testosterone in the metabolic syndrome: a review. J Steroid Biochem Mol Biol, 2009. 114(1-2): p. 40-3.
6. Ullah, M.I., et al., Testosterone deficiency as a risk factor for cardiovascular disease. Horm Metab Res, 2011. 43(3): p. 153-64.
7. Yeap, B.B., A.B. Araujo, and G.A. Wittert, Do low testosterone levels contribute to ill-health during male ageing? Crit Rev Clin Lab Sci, 2012. 49(5-6): p. 168-82.
8. Traish, A.M., et al., The dark side of testosterone deficiency: I. Metabolic syndrome and erectile dysfunction. J Androl, 2009. 30(1): p. 10-22.
9. Traish, A.M., et al., The dark side of testosterone deficiency: III. Cardiovascular disease. J Androl, 2009. 30(5): p. 477-94.
10. Traish, A.M., F. Saad, and A. Guay, The dark side of testosterone deficiency: II. Type 2 diabetes and insulin resistance. J Androl, 2009. 30(1): p. 23-32.
11. Traish, A.M., R. Abdou, and K.E. Kypreos, Androgen deficiency and atherosclerosis: The lipid link. Vascul Pharmacol, 2009. 51(5-6): p. 303-13.
12. Mesbah Oskui, P., et al., Testosterone and the cardiovascular system: a comprehensive review of the clinical literature. J Am Heart Assoc, 2013. 2(6): p. e000272.
13. Traish, A.M., Adverse health effects of testosterone deficiency (TD) in men. Steroids, 2014.
14. Buvat, J., et al., Endocrine aspects of male sexual dysfunctions. J Sex Med, 2010. 7(4 Pt 2): p. 1627-56.
15. Travison, T.G., et al., The relationship between libido and testosterone levels in aging men. J Clin Endocrinol Metab, 2006. 91(7): p. 2509-13.
16. Yassin, A.A. and F. Saad, Treatment of sexual dysfunction of hypogonadal patients with long-acting testosterone undecanoate (Nebido). World J Urol, 2006. 24(6): p. 639-44.
17. Yassin, A.A. and F. Saad, Improvement of sexual function in men with late-onset hypogonadism treated with testosterone only. J Sex Med, 2007. 4(2): p. 497-501.
18. Wu, F.C., et al., Identification of late-onset hypogonadism in middle-aged and elderly men. N Engl J Med, 2010. 363(2): p. 123-35.
19. Wu, F.C., et al., Hypothalamic-pituitary-testicular axis disruptions in older men are differentially linked to age and modifiable risk factors: the European Male Aging Study. J Clin Endocrinol Metab, 2008. 93(7): p. 2737-45.
20. Harkonen, K., et al., The polymorphic androgen receptor gene CAG repeat, pituitary-testicular function and andropausal symptoms in ageing men. Int J Androl, 2003. 26(3): p. 187-94.
21. van den Beld, A., et al., Luteinizing hormone and different genetic variants, as indicators of frailty in healthy elderly men. J Clin Endocrinol Metab, 1999. 84(4): p. 1334-9.
22. Tajar, A., et al., Characteristics of secondary, primary, and compensated hypogonadism in aging men: evidence from the European Male Ageing Study. J Clin Endocrinol Metab, 2010. 95(4): p. 1810-8.
23. Ohlsson, C., et al., High serum testosterone is associated with reduced risk of cardiovascular events in elderly men. The MrOS (Osteoporotic Fractures in Men) study in Sweden. J Am Coll Cardiol, 2011. 58(16): p. 1674-81.
24. Khaw, K.T., et al., Endogenous testosterone and mortality due to all causes, cardiovascular disease, and cancer in men: European prospective investigation into cancer in Norfolk (EPIC-Norfolk) Prospective Population Study. Circulation, 2007. 116(23): p. 2694-701.
25. Malkin, C.J., et al., Low serum testosterone and increased mortality in men with coronary heart disease. Heart, 2010. 96(22): p. 1821-5.
26. Traish, A.M., et al., Testosterone deficiency. Am J Med, 2011. 124(7): p. 578-87.






Monica….I enjoy reading your articles on the benefits of TRT. With so much negative press regarding the health risks associated with TRT, I still can’t figure out why there is not more adoption. You don’t see men with higher testosterone levels coming down with ailments. I myself was on TRT for roughly 9 months until my PSA started to increase which really spooked me. My doc suggested if it continues to rise, then we will stop it. I decided to stop myself. Your other article speaking to the “saturation point” and that an increase in PSA is a normal by product of TRT doesn’t mean an increase in prostate cancer. I am considering restarting TRT again working through my Urologist, but based upon what you know and have researched, I would like your opinion on which therapy is considered best. I was doing .5 ml injection every two weeks of a popular synthetic brand. All I’ve ever heard was negativity regarding the safety of putting something “synthetic” in to your body, but based upon everything I can find/read it appears to be safe. There is no natural or “bio-identical” form as both are made in a compounding facility. I know you are not an MD and can’t make recommendations on treatment, but what is your opinion on the long term use of the injectible form of TRT?
I’m glad to hear that Brandon. 🙂
You say you were on TRT for 9 months; did you PSA raise above the reference range? As I outlined in my article on the saturation point, an initial rise in PSA is a normal physiological response to initiation of TRT.
All testosterone medications are testosterone; the molecule is identical to endogenous testosterone. The issue of bioidentical vs synthetic does not apply to testosterone like it does to female estrogen/progesterone HRT.
With testosterone, the difference between preparations is the ester to which the testosterone is bound, which affects pharmacokinetics (ir half live in the blood stream). Once in the body, testosterone gets liberated from the ester. Long-acting esters like testosterone undecanoate (ie Aveed) is better for many men because it doesn’t cause supraphysiological spikes in T levels. Aveed therefore provides a more physiological treatment that is better for the prostate.
I have been on injections to reduce my body’s testosterone production for three years because of prostate cancer. At 82 years old, I certainly am affected on the sex side, but i continue to work out with weights and cardio three or four times per week. Can I expect the effects that you mention if I continue the treatment?
Thanks, Joe
The treatment you are on is called androgen deprivation therapy (ADT).
Yes, ADT is well known to induce multiple detrimental health effects, including those outlined in this article.
It is good that you keep working out, but you also need to monitor your health status with comprehensive blood test panels.
Monica / Will,
I have been an avid reader of the Brink Zone for the last 5 – 6 years and have followed your reports on TRT for a long time.
After battling with quite a number of GP’s here in Australia, I have just started my first course of TRT yesterday 8/9/14.
It’s largely thanks to you and Will, because I have been using your reports on the subject to push my case with the doctors. I have printed out your reports and physically taken them to the Doctors and stayed with them whilst reading and discussing them.
It has taken nearly 4 years to win the battle, but I got there.
Thanks to yourself and will.
You know what they say “Happy Wife = Happy life”
Jack
Jack, I am thrilled to hear that!
Congratulations to your victory!!
Yes enjoyed the article on Testosterone and this one altho kinda sci-fi to read I basically understood….Will can get real technical sometimes, he needs to dumb things down for people like me….LOL….
Don’t know what this means but have had my T count checked every couple of years and was always told it was ‘normal’…….So by chance I started using something called DHEA sublingually and noticed almost immediately (within several hours) a lift in more ways than one. I didnt know I had ED problems until I started this stuff and found out that I’ve been losing something gradually over the years and didnt know it…………..Havent felt like this since my 20s..and I’m over 60 now and quite fit…it was a real eye opener that something like this DHEA stuff had an impact on my body in this way…..I havent noticed any increase in workout stamina but as far as my manhood apparatus, its a hit. Maybe Will can address the usefulness of DHEA sometime or refer me to where he has already addressed.
Just paste “DHEA” in search 😛
I’m thankful for this article, Monica. Of all the ones I’ve read on the subject, this one put a scare into me. Some of those symptoms apply directly to me! I’m going to contact my primary doctor and get tested, to be absolutely sure of what I’m dealing with. Having sleep apnea since childhood hasn’t helped that situation, but I’ve been under therapy for that, since 2002.
You’re welcome Kent.
I’m glad the article impelled you to take action for your own health! 🙂
Hello, My name is Brett and just found this sight which comes at a good time because my blood tests for the last couple of months have come up low on testosterone. My doctor told me my free testosterone levels are 6.2 which he said should be over 7.0 but he said my total is not as bad. He asked how I feel and how is my energy and sexual performance which I said they have come down. He told me to try exercising more with weights but he also said my weight is good. He asked me if I wanted to take testosterone gels or the patch that kind of scared me so I told him I would workout. I did’nt tell him but I’m going to try this natural product called MAN GREENS BY CHAD HOUSE to see if my numbers go up. I would appreciate any advice on this subject. Thanks
I have no faith in OTC “T booster” supplements. I have a lengthy article on that topic here if you search for it.