Alleged concerns regarding risk of cardiovascular disease with testosterone replacement therapy (TRT) have been promulgated recently. However, a large and growing number of intervention studies show to the contrary that TRT reduces cardiovascular risk factors and confers multiple beneficial health effects. Thus, fears promoted by some recent flawed studies need to be critically re-evaluated.
This article gives an overview of studies that have investigated health effects and safety of TRT.[1] As outlined here, the position that testosterone deficiency (TD) should be regarded as a risk factor for cardiovascular disease is supported by a rapidly expanding body of evidence.[2-4]
In a previous article I outlines all detrimental health consequences of hypogonadism, aka testosterone deficiency or low-T:
In this article I will describe the effects of testosterone therapy (TRT) on a wide range of risk factors (some of which are relatively unknown).
Key effects of testosterone replacement therapy
* TRT has beneficial effects on body composition:
Increased muscle mass (size) / fat-free mass / lean body mass [5-20]
Reduced waist circumference and visceral fat mass [6, 7, 16, 21-42]
Reduced total body fat mass / percent body fat [5, 6, 8-12, 14, 17, 19, 20, 29, 43, 44]
Weight loss [23, 30, 33-39, 41, 45]
Improved muscle function and exercise capacity [9, 44, 46, 47]
* TRT has beneficial effects on lipid profile:
Reduced Total cholesterol (TC) [8, 31-34, 36, 41-43, 45, 48-50]
Reduced TC / HDL ratio [37]
Reduced LDL cholesterol [8, 33, 34, 36, 41-43, 49-51]
Reduced triglycerides (TGs) [24-26, 33, 34, 36, 41, 42, 45]
Reduced Lp(a) [49]
Increased HDL levels [24, 33, 34, 36, 41, 45, 51]
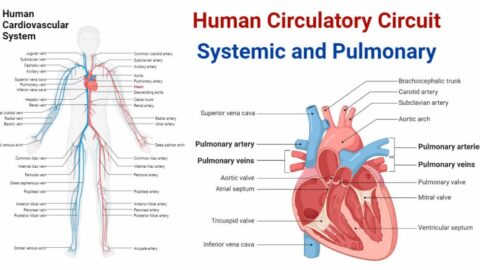
* TRT has beneficial effects on cardiovascular function:
Reduced arterial stiffness [13, 52]
Reduced CIMT (carotid intima media thickness) [28]
Reduced blood pressure [22, 33, 34, 36, 37, 40, 41]
Increased circulating endothelial progenitor cell (EPC) number [53]
Decreased levels of osteoprotegerin (a novel independent marker of cardiovascular risk) [54]
* TRT has beneficial effects on glucose metabolism, which reduce risk of diabetes:
Increased insulin sensitivity [7, 13, 14, 17, 19, 24, 25, 28, 31, 37, 39, 46, 49]
Reduced glucose levels [22, 24, 26, 30, 31, 33, 34, 36, 39, 41]
Reduced HbA1c levels [24, 30-34, 36, 37, 49]
* TRT has beneficial effects on inflammatory parameters:
Decreased levels of liver enzymes [34, 36]
Decreased CRP levels [21, 24, 28, 33, 34, 36, 55, 56]
Reduction in inflammatory cytokines (TNF-alpha and IL-1beta) [21, 48]
Increase in anti-inflammatory cytokines (IL-10) [48]
* TRT has beneficial effects on the skeleton:
Increased bone mineral density (BMD) [10, 12, 55, 57]
* TRT has beneficial effects on longevity:
Reduced risk of mortality and improved survival [58, 59]
* TRT has beneficial effects on sexual function:
Increased libido, improved erectile function and ejaculatory function [6, 11, 12, 29, 30, 38, 41-43, 49, 60-64]
* TRT has beneficial effects on quality of life:
Less fatigue and improvement in energy, mood, vitality [11, 12, 20, 38, 41, 42, 62, 65, 66]
* Several long-term registry studies confirm beneficial key effects: [23, 33, 35-37, 41, 67]
– TRT effectively restores physiological T levels within the first 12 months and these restored T levels are maintained with T therapy throughout the entire study period, which at this point is up to 6 years.
– Long-term TRT results in a marked and sustained reduction in body weight, waist circumference, BMI, CRP (C-reactive protein; an inflammatory biomarker), HbA1c and improves the lipid profile by reducing total cholesterol, LDL and triglycerides while increasing HDL.
– It is especially notable that the long-term reductions in body weight, waist circumference and HbA1c keep progressing throughout 5 years, and further improve after each year of TRT.
* Safety of TRT
– The most common side effects of TRT are increases in hematocrit and PSA.[42, 68] However, these elevations occur within the first 12 months, and thereafter remain stable with continued TRT for up to 5 years.[37] This corroborates findings from a previous 3 year-long study which demonstrated that elevations (within the reference range) of hemacocrit and PSA plateau at 12 months and 6 months respectively, after initiation of TRT.
– 5 years of TRT also does not change the International Prostate Symptom Score (IPSS), maximum urinary flow (Qmax) rate, post-void residual (PVR) volume, or prostate size.[69] Thus, long-term TRT does not impact negatively on lower urinary tract symptoms (LUTS) and prostate volume.
What is known
Ttosterone deficiency (TD), a.k.a hypogonadism, is a common clinical condition, affecting almost 40% of men aged 45 years and older.[70] Observational studies report associations of lower testosterone levels with poorer health outcomes in ageing men, including frailty, reduced sexual activity, insulin resistance, cognitive decline, cardiovascular events and mortality [71, 72]. Decreased testosterone levels also are associated with increased risks of osteoporosis, metabolic syndrome, type 2 diabetes. [73]
Men with the metabolic syndrome have lower testosterone levels than age-matched men without the metabolic syndrome [22, 74-78], and risk of developing the metabolic syndrome is lower in men with higher testosterone levels.[79-83] Similarly, men with type 2 diabetes have lower testosterone levels than men without a history of diabetes [84-90], and risk of type 2 diabetes is lower in men with high testosterone levels.[91-94] Likewise, men with coronary artery disease have lower testosterone levels than age-matched men without coronary artery disease [95, 96], and risk of cardiovascular events [97] and cardiovascular death [96] is lower in men with high testosterone levels.
What new studies show
A comprehensive review of TRT interventions confirms that TRT is safe if treatment and monitoring are appropriately executed. The evidence available to date does not support recently raised concerns about potential detrimental cardiovascular effects of testosterone therapy. Instead, a growing number of interventions studies show that TRT has multiple beneficial effects, as outlined above.
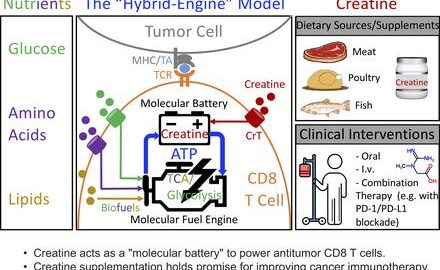
It is notable that TRT also has beneficial effects on novel risk factors like osteoprotegerin [54] and circulating (in the blood stream) endothelial progenitor cells (EPCs).[53] There is now emerging evidence that osteoprotegerin contributes to the development of atherosclerosis and cardiovascular diseases by amplifying the adverse effects of inflammation and several traditional risk factors, such as dyslipidemia, endothelial dysfunction, diabetes and hypertension.[98] This is supported by studies showing that severity of atherosclerosis is significantly associated with higher osteoprotegerin levels, and findings that osteoprotegerin is an independent predictor of cardiovascular events [99, 100] and heart disease. [99, 101] This being that case, it is interesting that TRT reduces osteoprotegerin levels.[54] Endothelial progenitor cells number is another relatively unknown health indicator.
The level of circulating endothelial progenitor cells, which play a critical role in repair of blood vessel injuries, has been shown to predict the occurrence of future cardiovascular events and death from cardiovascular causes.[102] In line with this, a reduced number of circulating endothelial progenitor cells is an independent predictor of atherosclerosis progression. [103] Low levels of testosterone are associated with a low number of circulating endothelial progenitor cells [104] and testosterone replacement therapy has been demonstrated to induce an increase in circulating endothelial progenitor cell number, possibly via a direct effect on the bone marrow.[53, 104] Emerging research shows that testosterone an important role in the development and maturation of endothelial progenitor cells, and regulates vascular (endothelial) function.[105] Because of the critical role of the inner lining of blood vessels (aka endothelium) in regulating erectile function, a better understanding of the function of endothelial progenitor cells may pave the way to development of new therapeutic approaches for the treatment of erectile dysfunction.[105]
Thus, there is now ample evidence to argue that TD should be an element in the definition of the metabolic syndrome.[106] In the long run, the beneficial effects of TRT on the metabolic parameters outlined above would protect against development of the main killers; cardiovascular disease and type-2 diabetes. There is a high prevalence of TD in type-2 diabetics [84-90], and because multiple studies demonstrate metabolic benefits of TRT in type-2 diabetic patients [24, 30, 31, 45, 49, 107] it has been suggested that testosterone supplementation be regarded as a new therapy for diabetes.[108] There is also mounting data to support use of TRT in treatment of obesity. [23, 33, 35-37, 41, 67, 109, 110]
Low testosterone levels together with standard risk factors can be used to improved health risk prediction, and may represent a valuable biomarker for indication of cardiovascular disease risk.[111] Due to the strong associations of low testosterone levels with detrimental health outcomes, it is likely that TD contributes, at least partly, to aging related health deterioration. It has therefore been suggested that testosterone deficiency should be regarded as a risk factor for cardiovascular disease.[2-4]

References:
1. Traish, A.M., Outcomes of testosterone therapy in men with testosterone deficiency (TD): Part II. Steroids, 2014.
2. Ullah, M.I., et al., Testosterone deficiency as a risk factor for cardiovascular disease. Horm Metab Res, 2011. 43(3): p. 153-64.
3. Jones, T.H., Testosterone deficiency: a risk factor for cardiovascular disease? Trends Endocrinol Metab, 2010. 21(8): p. 496-503.
4. Maggio, M. and S. Basaria, Welcoming low testosterone as a cardiovascular risk factor. Int J Impot Res, 2009. 21(4): p. 261-4.
5. Bhasin, S., et al., Effect of testosterone supplementation with and without a dual 5alpha-reductase inhibitor on fat-free mass in men with suppressed testosterone production: a randomized controlled trial. JAMA, 2012. 307(9): p. 931-9.
6. Finkelstein, J.S., et al., Gonadal steroids and body composition, strength, and sexual function in men. N Engl J Med, 2013. 369(11): p. 1011-22.
7. Marin, P., M. Krotkiewski, and P. Bjorntorp, Androgen treatment of middle-aged, obese men: effects on metabolism, muscle and adipose tissues. Eur J Med, 1992. 1(6): p. 329-36.
8. Page, S.T., et al., Exogenous testosterone (T) alone or with finasteride increases physical performance, grip strength, and lean body mass in older men with low serum T. J Clin Endocrinol Metab, 2005. 90(3): p. 1502-10.
9. Srinivas-Shankar, U., et al., Effects of testosterone on muscle strength, physical function, body composition, and quality of life in intermediate-frail and frail elderly men: a randomized, double-blind, placebo-controlled study. J Clin Endocrinol Metab, 2010. 95(2): p. 639-50.
10. Svartberg, J., et al., Testosterone treatment in elderly men with subnormal testosterone levels improves body composition and BMD in the hip. Int J Impot Res, 2008. 20(4): p. 378-87.
11. Wang, C., et al., Transdermal testosterone gel improves sexual function, mood, muscle strength, and body composition parameters in hypogonadal men. J Clin Endocrinol Metab, 2000. 85(8): p. 2839-53.
12. Wang, C., et al., Long-term testosterone gel (AndroGel) treatment maintains beneficial effects on sexual function and mood, lean and fat mass, and bone mineral density in hypogonadal men. J Clin Endocrinol Metab, 2004. 89(5): p. 2085-98.
13. Hoyos, C.M., et al., Body compositional and cardiometabolic effects of testosterone therapy in obese men with severe obstructive sleep apnoea: a randomised placebo-controlled trial. Eur J Endocrinol, 2012. 167(4): p. 531-41.
14. Naharci, M.I., et al., Effect of testosterone on insulin sensitivity in men with idiopathic hypogonadotropic hypogonadism. Endocr Pract, 2007. 13(6): p. 629-35.
15. Brodsky, I.G., P. Balagopal, and K.S. Nair, Effects of testosterone replacement on muscle mass and muscle protein synthesis in hypogonadal men–a clinical research center study. J Clin Endocrinol Metab, 1996. 81(10): p. 3469-75.
16. Allan, C.A., et al., Testosterone therapy prevents gain in visceral adipose tissue and loss of skeletal muscle in nonobese aging men. J Clin Endocrinol Metab, 2008. 93(1): p. 139-46.
17. Malkin, C.J., T.H. Jones, and K.S. Channer, The effect of testosterone on insulin sensitivity in men with heart failure. Eur J Heart Fail, 2007. 9(1): p. 44-50.
18. Frederiksen, L., et al., Testosterone therapy increased muscle mass and lipid oxidation in aging men. Age (Dordr), 2012. 34(1): p. 145-56.
19. Juang, P.S., et al., Testosterone with dutasteride, but not anastrazole, improves insulin sensitivity in young obese men: a randomized controlled trial. J Sex Med, 2014. 11(2): p. 563-73.
20. Behre, H.M., et al., A randomized, double-blind, placebo-controlled trial of testosterone gel on body composition and health-related quality-of-life in men with hypogonadal to low-normal levels of serum testosterone and symptoms of androgen deficiency over 6 months with 12 months open-label follow-up. Aging Male, 2012. 15(4): p. 198-207.
21. Kalinchenko, S.Y., et al., Effects of testosterone supplementation on markers of the metabolic syndrome and inflammation in hypogonadal men with the metabolic syndrome: the double-blinded placebo-controlled Moscow study. Clin Endocrinol (Oxf), 2010. 73(5): p. 602-12.
22. Bhattacharya, R.K., et al., Effect of 12 months of testosterone replacement therapy on metabolic syndrome components in hypogonadal men: data from the Testim Registry in the US (TRiUS). BMC Endocr Disord, 2011. 11: p. 18.
23. Saad, F., et al., Long-term treatment of hypogonadal men with testosterone produces substantial and sustained weight loss. Obesity (Silver Spring), 2013. 21(10): p. 1975-81.
24. Heufelder, A.E., et al., Fifty-two-week treatment with diet and exercise plus transdermal testosterone reverses the metabolic syndrome and improves glycemic control in men with newly diagnosed type 2 diabetes and subnormal plasma testosterone. J Androl, 2009. 30(6): p. 726-33.
25. Marin, P., Testosterone and regional fat distribution. Obes Res, 1995. 3 Suppl 4: p. 609S-612S.
26. Marin, P., et al., Androgen treatment of abdominally obese men. Obes Res, 1993. 1(4): p. 245-51.
27. Marin, P., et al., Assimilation of triglycerides in subcutaneous and intraabdominal adipose tissues in vivo in men: effects of testosterone. J Clin Endocrinol Metab, 1996. 81(3): p. 1018-22.
28. Aversa, A., et al., Effects of testosterone undecanoate on cardiovascular risk factors and atherosclerosis in middle-aged men with late-onset hypogonadism and metabolic syndrome: results from a 24-month, randomized, double-blind, placebo-controlled study. J Sex Med, 2010. 7(10): p. 3495-503.
29. Aversa, A., et al., Efficacy and safety of two different testosterone undecanoate formulations in hypogonadal men with metabolic syndrome. J Endocrinol Invest, 2010. 33(11): p. 776-83.
30. Boyanov, M.A., Z. Boneva, and V.G. Christov, Testosterone supplementation in men with type 2 diabetes, visceral obesity and partial androgen deficiency. Aging Male, 2003. 6(1): p. 1-7.
31. Kapoor, D., et al., Testosterone replacement therapy improves insulin resistance, glycaemic control, visceral adiposity and hypercholesterolaemia in hypogonadal men with type 2 diabetes. Eur J Endocrinol, 2006. 154(6): p. 899-906.
32. Hackett, G., et al., Testosterone replacement therapy improves metabolic parameters in hypogonadal men with type 2 diabetes but not in men with coexisting depression: the BLAST study. J Sex Med, 2014. 11(3): p. 840-56.
33. Haider, A., et al., Hypogonadal obese men with and without diabetes mellitus type 2 lose weight and show improvement in cardiovascular risk factors when treated with testosterone: an observational study. . Obes Res Clin Pract 2013.
34. Haider, A., et al., Effects of Long-Term Testosterone Therapy on Patients with “Diabesity”: Results of Observational Studies of Pooled Analyses in Obese Hypogonadal Men with Type 2 Diabetes. International Journal of Endocrinology, 2014: p. Article ID 683515.
35. Yassin, A. and G. Doros, Testosterone therapy in hypogonadal men results in sustained and clinically meaningful weight loss. Clin Obes, 2013. 3(3-4): p. 73-83.
36. Traish, A.M., et al., Long-term testosterone therapy in hypogonadal men ameliorates elements of the metabolic syndrome: an observational, long-term registry study. Int J Clin Pract, 2014. 68(3): p. 314-29.
37. Francomano, D., A. Lenzi, and A. Aversa, Effects of five-year treatment with testosterone undecanoate on metabolic and hormonal parameters in ageing men with metabolic syndrome. Int J Endocrinol, 2014. 2014: p. 527470.
38. Pexman-Fieth, C., et al., A 6-month observational study of energy, sexual desire, and body proportions in hypogonadal men treated with a testosterone 1% gel. Aging Male, 2014. 17(1): p. 1-11.
39. Strollo, F., et al., Low-intermediate dose testosterone replacement therapy by different pharmaceutical preparations improves frailty score in elderly hypogonadal hyperglycaemic patients. Aging Male, 2013. 16(2): p. 33-7.
40. Li, J.Y., et al., Effects of androgen supplementation therapy on partial androgen deficiency in the aging male: a preliminary study. Aging Male, 2002. 5(1): p. 47-51.
41. Yassin, D.J., et al., Long-term testosterone treatment in elderly men with hypogonadism and erectile dysfunction reduces obesity parameters and improves metabolic syndrome and health-related quality of life. J Sex Med, 2014. 11(6): p. 1567-76.
42. Zitzmann, M., et al., IPASS: a study on the tolerability and effectiveness of injectable testosterone undecanoate for the treatment of male hypogonadism in a worldwide sample of 1,438 men. J Sex Med, 2013. 10(2): p. 579-88.
43. Permpongkosol, S., N. Tantirangsee, and K. Ratana-olarn, Treatment of 161 men with symptomatic late onset hypogonadism with long-acting parenteral testosterone undecanoate: effects on body composition, lipids, and psychosexual complaints. J Sex Med, 2010. 7(11): p. 3765-74.
44. Stout, M., et al., Testosterone therapy during exercise rehabilitation in male patients with chronic heart failure who have low testosterone status: a double-blind randomized controlled feasibility study. Am Heart J, 2012. 164(6): p. 893-901.
45. Mitkov, M.D., I.Y. Aleksandrova, and M.M. Orbetzova, Effect of transdermal testosterone or alpha-lipoic acid on erectile dysfunction and quality of life in patients with type 2 diabetes mellitus. Folia Med (Plovdiv), 2013. 55(1): p. 55-63.
46. Caminiti, G., et al., Effect of long-acting testosterone treatment on functional exercise capacity, skeletal muscle performance, insulin resistance, and baroreflex sensitivity in elderly patients with chronic heart failure a double-blind, placebo-controlled, randomized study. J Am Coll Cardiol, 2009. 54(10): p. 919-27.
47. Ferrando, A.A., et al., Testosterone administration to older men improves muscle function: molecular and physiological mechanisms. Am J Physiol Endocrinol Metab, 2002. 282(3): p. E601-7.
48. Malkin, C.J., et al., The effect of testosterone replacement on endogenous inflammatory cytokines and lipid profiles in hypogonadal men. J Clin Endocrinol Metab, 2004. 89(7): p. 3313-8.
49. Jones, T.H., et al., Testosterone replacement in hypogonadal men with type 2 diabetes and/or metabolic syndrome (the TIMES2 study). Diabetes Care, 2011. 34(4): p. 828-37.
50. Zgliczynski, S., et al., Effect of testosterone replacement therapy on lipids and lipoproteins in hypogonadal and elderly men. Atherosclerosis, 1996. 121(1): p. 35-43.
51. Zitzmann, M. and E. Nieschlag, Androgen receptor gene CAG repeat length and body mass index modulate the safety of long-term intramuscular testosterone undecanoate therapy in hypogonadal men. J Clin Endocrinol Metab, 2007. 92(10): p. 3844-53.
52. Yaron, M., et al., Effect of testosterone replacement therapy on arterial stiffness in older hypogonadal men. Eur J Endocrinol, 2009. 160(5): p. 839-46.
53. Liao, C.H., et al., Testosterone replacement therapy can increase circulating endothelial progenitor cell number in men with late onset hypogonadism. Andrology, 2013. 1(4): p. 563-9.
54. Frederiksen, L., et al., Osteoprotegerin levels decrease during testosterone therapy in aging men and are associated with changed distribution of regional fat. Horm Metab Res, 2013. 45(4): p. 308-13.
55. Aversa, A., et al., Effects of long-acting testosterone undecanoate on bone mineral density in middle-aged men with late-onset hypogonadism and metabolic syndrome: results from a 36 months controlled study. Aging Male, 2012. 15(2): p. 96-102.
56. Kapoor, D., et al., The effect of testosterone replacement therapy on adipocytokines and C-reactive protein in hypogonadal men with type 2 diabetes. Eur J Endocrinol, 2007. 156(5): p. 595-602.
57. Wang, C., et al., Effects of transdermal testosterone gel on bone turnover markers and bone mineral density in hypogonadal men. Clin Endocrinol (Oxf), 2001. 54(6): p. 739-50.
58. Shores, M.M., et al., Testosterone treatment and mortality in men with low testosterone levels. J Clin Endocrinol Metab, 2012. 97(6): p. 2050-8.
59. Muraleedharan, V., et al., Testosterone deficiency is associated with increased risk of mortality and testosterone replacement improves survival in men with type 2 diabetes. Eur J Endocrinol, 2013. 169(6): p. 725-33.
60. Bolona, E.R., et al., Testosterone use in men with sexual dysfunction: a systematic review and meta-analysis of randomized placebo-controlled trials. Mayo Clin Proc, 2007. 82(1): p. 20-8.
61. Allan, C.A., et al., Testosterone therapy increases sexual desire in ageing men with low-normal testosterone levels and symptoms of androgen deficiency. Int J Impot Res, 2008. 20(4): p. 396-401.
62. Hackett, G., et al., Testosterone replacement therapy with long-acting testosterone undecanoate improves sexual function and quality-of-life parameters vs. placebo in a population of men with type 2 diabetes. J Sex Med, 2013. 10(6): p. 1612-27.
63. Amiaz, R., et al., Testosterone gel replacement improves sexual function in depressed men taking serotonergic antidepressants: a randomized, placebo-controlled clinical trial. J Sex Marital Ther, 2011. 37(4): p. 243-54.
64. Corona, G., et al., Testosterone supplementation and sexual function: a meta-analysis study. J Sex Med, 2014. 11(6): p. 1577-92.
65. Tong, S.F., et al., Effect of long-acting testosterone undecanoate treatment on quality of life in men with testosterone deficiency syndrome: a double blind randomized controlled trial. Asian J Androl, 2012. 14(4): p. 604-11.
66. Ho, C.C., et al., A randomized, double-blind, placebo-controlled trial on the effect of long-acting testosterone treatment as assessed by the Aging Male Symptoms scale. BJU Int, 2012. 110(2): p. 260-5.
67. Haider, A., et al., Effects of long-term testosterone therapy on patients with “diabesity”: results of observational studies of pooled analyses in obese hypogonadal men with type 2 diabetes. Int J Endocrinol, 2014. 2014: p. 683515.
68. Bhasin, S., et al., Testosterone therapy in men with androgen deficiency syndromes: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab, 2010. 95(6): p. 2536-59.
69. Francomano, D., et al., Effects of 5-year treatment with testosterone undecanoate on lower urinary tract symptoms in obese men with hypogonadism and metabolic syndrome. Urology, 2014. 83(1): p. 167-73.
70. Mulligan, T., et al., Prevalence of hypogonadism in males aged at least 45 years: the HIM study. Int J Clin Pract, 2006. 60(7): p. 762-9.
71. Yeap, B.B., A.B. Araujo, and G.A. Wittert, Do low testosterone levels contribute to ill-health during male ageing? Crit Rev Clin Lab Sci, 2012. 49(5-6): p. 168-82.
72. Yeap, B.B., Are declining testosterone levels a major risk factor for ill-health in aging men? Int J Impot Res, 2009. 21(1): p. 24-36.
73. Yeap, B.B., Testosterone and ill-health in aging men. Nat Clin Pract Endocrinol Metab, 2009. 5(2): p. 113-21.
74. Singh, S.K., R. Goyal, and D.D. Pratyush, Is hypoandrogenemia a component of metabolic syndrome in males? Exp Clin Endocrinol Diabetes, 2011. 119(1): p. 30-5.
75. Maggio, M., et al., Association between hormones and metabolic syndrome in older Italian men. J Am Geriatr Soc, 2006. 54(12): p. 1832-8.
76. Garcia-Cruz, E., et al., Metabolic syndrome in men with low testosterone levels: relationship with cardiovascular risk factors and comorbidities and with erectile dysfunction. J Sex Med, 2013. 10(10): p. 2529-38.
77. Grosman, H., et al., Association between testosterone levels and the metabolic syndrome in adult men. Aging Male, 2014: p. 1-5.
78. Yeap, B.B., et al., Differential associations of testosterone, dihydrotestosterone and oestradiol with physical, metabolic and health-related factors in community-dwelling men aged 17-97 years from the Busselton Health Survey. Clin Endocrinol (Oxf), 2014. 81(1): p. 100-8.
79. Kupelian, V., et al., Low sex hormone-binding globulin, total testosterone, and symptomatic androgen deficiency are associated with development of the metabolic syndrome in nonobese men. J Clin Endocrinol Metab, 2006. 91(3): p. 843-50.
80. Rodriguez, A., et al., Aging, androgens, and the metabolic syndrome in a longitudinal study of aging. J Clin Endocrinol Metab, 2007. 92(9): p. 3568-72.
81. Tsujimura, A., et al., Is low testosterone concentration a risk factor for metabolic syndrome in healthy middle-aged men? Urology, 2013. 82(4): p. 814-9.
82. Tong, P.C., et al., Association of testosterone, insulin-like growth factor-I, and C-reactive protein with metabolic syndrome in Chinese middle-aged men with a family history of type 2 diabetes. J Clin Endocrinol Metab, 2005. 90(12): p. 6418-23.
83. Haring, R., et al., Prediction of metabolic syndrome by low serum testosterone levels in men: results from the study of health in Pomerania. Diabetes, 2009. 58(9): p. 2027-31.
84. Grossmann, M., et al., Low testosterone levels are common and associated with insulin resistance in men with diabetes. J Clin Endocrinol Metab, 2008. 93(5): p. 1834-40.
85. Chandel, A., et al., Testosterone concentration in young patients with diabetes. Diabetes Care, 2008. 31(10): p. 2013-7.
86. Hernandez-Mijares, A., et al., Testosterone levels in males with type 2 diabetes and their relationship with cardiovascular risk factors and cardiovascular disease. J Sex Med, 2010. 7(5): p. 1954-64.
87. Dhindsa, S., et al., Testosterone concentrations in diabetic and nondiabetic obese men. Diabetes Care, 2010. 33(6): p. 1186-92.
88. Anderson, S.G., et al., Screening for hypogonadism in diabetes 2008/9: results from the Cheshire Primary Care cohort. Prim Care Diabetes, 2012. 6(2): p. 143-8.
89. Ogbera, O.A., et al., Hypogonadism and subnormal total testosterone levels in men with type 2 diabetes mellitus. J Coll Physicians Surg Pak, 2011. 21(9): p. 517-21.
90. Dhindsa, S., et al., Frequent occurrence of hypogonadotropic hypogonadism in type 2 diabetes. J Clin Endocrinol Metab, 2004. 89(11): p. 5462-8.
91. Ding, E.L., et al., Sex differences of endogenous sex hormones and risk of type 2 diabetes: a systematic review and meta-analysis. JAMA, 2006. 295(11): p. 1288-99.
92. Vikan, T., et al., Low testosterone and sex hormone-binding globulin levels and high estradiol levels are independent predictors of type 2 diabetes in men. Eur J Endocrinol, 2010. 162(4): p. 747-54.
93. Oh, J.Y., et al., Endogenous sex hormones and the development of type 2 diabetes in older men and women: the Rancho Bernardo study. Diabetes Care, 2002. 25(1): p. 55-60.
94. Stellato, R.K., et al., Testosterone, sex hormone-binding globulin, and the development of type 2 diabetes in middle-aged men: prospective results from the Massachusetts male aging study. Diabetes Care, 2000. 23(4): p. 490-4.
95. English, K.M., et al., Men with coronary artery disease have lower levels of androgens than men with normal coronary angiograms. Eur Heart J, 2000. 21(11): p. 890-4.
96. Malkin, C.J., et al., Low serum testosterone and increased mortality in men with coronary heart disease. Heart, 2010. 96(22): p. 1821-5.
97. Ohlsson, C., et al., High serum testosterone is associated with reduced risk of cardiovascular events in elderly men. The MrOS (Osteoporotic Fractures in Men) study in Sweden. J Am Coll Cardiol, 2011. 58(16): p. 1674-81.
98. Montagnana, M., et al., The role of osteoprotegerin in cardiovascular disease. Ann Med, 2013. 45(3): p. 254-64.
99. Davenport, C., et al., Identifying coronary artery disease in men with type 2 diabetes: osteoprotegerin, pulse wave velocity, and other biomarkers of cardiovascular risk. J Hypertens, 2011. 29(12): p. 2469-75.
100. Livaudais, J.C., et al., Educating Hispanic women about breast cancer prevention: evaluation of a home-based promotora-led intervention. J Womens Health (Larchmt), 2010. 19(11): p. 2049-56.
101. Vik, A., et al., Serum osteoprotegerin is a predictor for incident cardiovascular disease and mortality in a general population: the Tromso Study. J Thromb Haemost, 2011. 9(4): p. 638-44.
102. Werner, N., et al., Circulating endothelial progenitor cells and cardiovascular outcomes. N Engl J Med, 2005. 353(10): p. 999-1007.
103. Schmidt-Lucke, C., et al., Reduced number of circulating endothelial progenitor cells predicts future cardiovascular events: proof of concept for the clinical importance of endogenous vascular repair. Circulation, 2005. 111(22): p. 2981-7.
104. Foresta, C., et al., Reduced number of circulating endothelial progenitor cells in hypogonadal men. J Clin Endocrinol Metab, 2006. 91(11): p. 4599-602.
105. Traish, A.M. and A. Galoosian, Androgens modulate endothelial function and endothelial progenitor cells in erectile physiology. Korean J Urol, 2013. 54(11): p. 721-31.
106. Saad, F. and L. Gooren, The role of testosterone in the metabolic syndrome: a review. J Steroid Biochem Mol Biol, 2009. 114(1-2): p. 40-3.
107. Cai, X., et al., Metabolic effects of testosterone replacement therapy on hypogonadal men with type 2 diabetes mellitus: a systematic review and meta-analysis of randomized controlled trials. Asian J Androl, 2014. 16(1): p. 146-52.
108. Corona, G., et al., Following the common association between testosterone deficiency and diabetes mellitus, can testosterone be regarded as a new therapy for diabetes? Int J Androl, 2009. 32(5): p. 431-41.
109. Saad, F., et al., Testosterone as potential effective therapy in treatment of obesity in men with testosterone deficiency: a review. Curr Diabetes Rev, 2012. 8(2): p. 131-43.
110. Saad, F. and L.J. Gooren, The role of testosterone in the etiology and treatment of obesity, the metabolic syndrome, and diabetes mellitus type 2. J Obes, 2011. 2011.
111. Vlachopoulos, C., et al., Plasma total testosterone and incident cardiovascular events in hypertensive patients. Am J Hypertens, 2013. 26(3): p. 373-81.





Excellent information Monica. I have been following your posts about TRT some time now. I have a question for you if you have any information or experience with. I basically am on TRT. T enanthate shots. I have tried every 3.5 days protocol, every other day protocol and have done multiple blood tests. My issue is i am trying to avoid an AI like arimidex.
My guess, my tests and my research are all telling me there is no way around this being on TRT without an AI also. I am talking about me and not in general. I know some lucky ones that do not aromatase anything!
I am in my 30s and my pre TRT estradiol or E2 was alread 38. I am guessing this due to our estrogen dominated world we live in. All xeno estrogens, plastics, tooth pastes, deoderants etc are all increasing are estradiol and that is why men are becoming women and we see so many young people suffer from low t. Whenever my T goes over 500 then i my E2 increases to 50-60pg/ml which in return makes me feel pretty shit.
Sorry for my blabber. Basically if you know any proven supplements or any information on how to avoid an AI with TRT for someone with already pre existing high E2 i would be very grateful for any information.
Thanks
Thank you! 🙂
The best way to avoid E2 elevation with TRT is to use testosterone preparations that do not cause supra-physiological spikes and fluctuations in T levels. I suggest you try Aveed (testosterone undecanoate) which is a long-acting ester and therefore only needs injecting every 6 wk. Transdermal T gel is another alternative.
What is the reason for your wanting to avoid AIs?
Thanks for the reply. Much appreciated Monica.
The reason i want to avoid AIs is because there are no long term studies on them especially on use on men. Right? Also many TRT doctors avoid them saying that the can lower IGF1 and mess with estrogen brain chemistry. Yes most claims are not supported by research.
Also because i am still young i would like to avoid taking another pharmaceutical for the rest of my life if possible. And the other reason is i cant seem to find the balance!!! I bought the best pill cutter and still cant cut them in exact 1/4. From my understanding the best way to take an AI is EOD protocol due to its half life. I have decided to try and dissolve them in vodka with a dropper. Hopefully that will work.
Any information/feedback is well appreciated. Thanks
To my knowledge there is only one study showing a reduction in IGF-1 level with arimidex. However, this was a short-term study in teenage boys, which makes it of questionable relevance to adult men… In women, arimidex actually increases blood IGF-1 levels…ultimately thought, it is not blood IGF-1 levels that are intersting, but intracelluar IGF-1 levels, especially in muscle and bone cells.
The risk with arimidex is that it very potently lowers estrogen, and when that happens, it increases risk for cognitive issue and loss of bone mineral density. The ideal E2 level is around I’d say 20-40.
Vodka is NOT a good idea! Ask your doctor for a lower dose pill.
How old are you and what are your total and free T levels?
I am 27 years old Monica and for the past 7 years all my blood tests for total T were at 360 ng/dl or and lower. My free T which was calculated by taking SHGB and albumin into account has been around 7.52 ng/dl.
The story is long, I will not bore you keep it short. I was a student living in UK when I was first diagnosed with low T and high prolactin (20 pg/ml). I did brain scan many times no adenoma was treated with dostinex and parlodel and prolactin fell to 14 pg/ml and has remained there for the past 4-5 years. I tried experimenting with lowering it but no real change and did not change my T. I had all lot of symptoms still after finishing with dostinex so I started visited doctors. Fatigue, mood swings, muscle weakness, libido issues, ED issues. Doctors in my country (way behind in HRT/TRT) said I am perfectly fine and my testosterone is perfectly fine and healthy. In UK they were going to treat but it was 2 late because I finished my studies and returned back to my country. I started doing my own research, read the book called testosterone a mans guide 2nd edition + testosterone syndrome by Eugene shippen and I spend hundreds of hours online reading on different stories and TRT.
Visited more doctors, endocrinologists, neurologists did a bunch of tests and MRIs. Everything clean, symptoms still there. Clearly this had to with my low T and medium estrogen (pre trt 38 pg/ml). I did all necessary tests before trt like full blood panel, full thyroid panel, dhea-s etc. I found good sources and started treatment on my own until I save some serious cash and visit an anti ageing clinic in US or UK. One doctor that owns a blood tests lab knows what I am doing and allows me to do all my tests there and gives his opinion but the choices are mine.
So I don’t have the option of asking for lower dosed pill. The only thing I could find online was mixing the pill in alcohol to dose more accurately. At the moment my Total T is at 830 ng/dl and my e2 at 60 pg/ml on an EOD protocol of 32 mg test. My free t at 19ng/dl I went from e3d protocol to eod hoping I can ditch the arimidex but no. I am going to lower test dose and start on low dose arimidex. Prob 0.25 arimidex with the test EOD. Btw massive change in every aspect of my life since starting TRT . I am just struggling to find balance with estrogen and have good and bad days.
Sorry for the long message, thanks for your input
John, there is not much room here in the comment section for long posts.
Feel free to email me if you have further questions:
Monica@MuscleNutrition.Fitness
Monica…I too have been following your articles and have found them very informative. I’ve even shared your studies with my own PCP and he is old school, but thankfully my Urologist is on board. Now that we know that TRT is safe and has been proven multiple times over the last 50 years to provide verifiable benefits, I have a question.
What are your thoughts on bioidentical testosterone vs synthetic testosterone? In my case, I am using Depo-Testosterone Cypionate intramuscular 100 mg every two weeks. That might be a whole other article in itself, but would appreciate your insight.
To start with, there is no such things as “bioidentical testosterone”!
Is kill this myth here:
http://www.agelessforever.net/bioidentical-estrogen-progesterone-hrt/what-are-bioidentical-hormones
Monica,
I am responding to the NEJM post you did earlier today. When reading through the comments, I ran across this statement and would like your opinion. “Bio-identical hormones: If one can boost their testosterone level naturally via exercise and weight loss that is wonderful and preferred. However, if one goes the replacement route, bio-identical hormones should be used (ie no pharmaceutical brand names as they are changed hormones in order to receive patents). Non bio-identical hormones all have different risks of stroke, DVT/PE and MI (though not proven with certainty as noted above in other’s comments), however, testosterone that is bio-identical reduces risks of MI, strokes and DVT/PE’s.
It is my understanding that Bio-Identical TRT is done by a compounding facility that is not regulated by the FDA. However, I was wondering if the compounding facility is able to custom manufacture TRT according to your specific blood work? Alternatively, are both the same in the end?
Brandon, please post your comment on the correct page http://www.brinkzone.com/anti-aging-and-hrt/for-or-against-testosterone-replacement-therapy-cast-your-vote/ and I will reply to your there. Thank you.
Hey im no professional and cant comment on the bioidentical question but i can comment on your dosage. 100mg every two weeks is a poor choice in my opinion and from all the research i have done. Half lives dont work exactly like on paper. For example when i take 60mg of test enathate that has a slightly shorter half life then cyprionate after 3 days my levels start to fall big time. Your starting protocol should be 80-100 mg a week in 2-3 doses or 1 dose worst case scenario. 100 every two weeks is very poor and after a week your levels will be VERY low if you ask me. If the doctor is going to use a useless protocol like that he should at least give 200mg for two weeks and still that is not ideal due to the spike you will get.
John
Yes, 100 mg every two weeks is likely sub-optimal for most men.
If you don’t like frequent injections, testosterone undecanoate (Aveed) is a good alternative as it is a long-acting ester that does not cause the supraphysiological spikes seen with enanthate and cypionate.
Ultimately however, it is the final target level achieved that matters; two men can achieve greatly different final T levels using the same T preparation and dose
Brandon, I cover the topic of “bio identical” T in a vid on the site here:
http://www.brinkzone.com/general-health/bio-identical-testosterone-the-facts/
Very nice, concise summary; suggest readers also clicking to W.Brink vid in re the ‘bioidentical testosterone’ scam (as well as his take on testosterone “boosters”. DJS MD,JD
Monica, I want to thank you for our extensive research and articulate presentations of TRT. I’ve been reading them avidly for some time now. I’m 66 years old and have kept myself in relatively good shape. Up till about a year ago my natural T level was adequate, albeit “low”. However, about a year ago, due to external stressors and age, my T level went down several notches. I requested beginning TRT with my MD who refused citing, as you suggest, cardiovascular risks. Despite my providing significant documentation to the contrary my MD persisted in her refusal to the point she eventually terminated our Dr./Patient relationship. Since then I’ve been searching for an appropriate, medically supervised, TRT regimen. Although I haven’t begun it yet, I intend to by the end of November (2014) — provided clearance from my cardiologist. It will be happy to come back and add my personal comments regarding the results of the treatment at that time. In the mean time, I want to thank you again for these helpful, well researched and documented articles.
I am glad to hear you are being proactive and taking charge of your own health. As you experienced, most mainstream doctors are not aware of the benefits of treating low-T, and the dangers of denying a patient with low-T testosterone therapy. As I have described in a previous article, most doctors still adhere to the T-prostate cancer myth. And more recently, flawed studies added heart diseases to the discussion.
Eventually the truth will come out; several medical research papers are in the process of getting published in peer-review medical journals. In the meantime, it is critical that men stay informed and seek out doctors who care more their patient’s health than preconceived dogma.
The key with TRT is to do regular blood test, before starting and then regular follow-ups to monitor all parameters, including:
total and free T
total and free estradiol
SHBG
PSA
IGF-1 and IGFBG-3
advanced lipid panel (to get info on all sub-fractions of LDL and HDL)
+ waist circumference
If you are hypogonadal; all these parameters will improve. Note that an initial PSA elevation is a natural response upon initiation of TRT; your PSA will then stabilize in a bit higher level after having reached the saturation point; but still within the reference range. Adherence and long-term perspective is key to derive maximal benefits of TRT.
For more info, check out: http://www.agelessforever.net/anti-aging-news-blog
Will & Monica,
What is a typical TRT dosage given in these studies I have
Perhaps that is something that can’e be included in such an article
I am just wondering if a guy using a rather large amount will continue to have positive results
What matters is not the dosage per see (which varied depending on T formulation), but the final T level achieved, and elevation in T level over baseline.
The reason for this is that two men given the exact same dose of the same T preparation can achieve very different different final T levels. This is why it is so important to titrate the dose based on your blood work and on your individual response.
Yes, as long as your stay within your optimal level (which has to be individually defined by regular blood work) you will be continuing to experience the benefits.
A good way to find your individual optimal T level is to reach the point right before your HDL starts to sink.
I am very interested in finding out if others are having the same problem. doctors seem to not believe that vitamin d is all that important for our levels to be at the optimum. I have read that normal is now lowered to20dl but it used to be 30dl. and the best levels are between 50 and 80. What is the correct answer scientifically. why are doctors not so interested in maintaining a vitamin D level between 50 and 80. Is this really hard to reach or do doctors know something they do not want the public to know?
Vitamin D deficiency does have a negative impact on T levels in men; and going from a vitamin D deficient state (below 20) to an optimal of 60-80 will elevate T levels in most cases.
One reason most doctors neglect of this is that medical school is not teaching nutrition; mainstream doctors practice what they were thought in med school. They either don’t have time, or don’t care, to stay up-to-date on new research findings. They often think nutrition and health promotion is not their business. As many doctors get commission from big pharma to prescribe drugs, it is more lucrative and time-efficient for them to wait until you get sick and then just reach for the prescription pad.
I’m in the process of getting my T-level checked out and, if I had any reservations about the therapy, they are long-gone. Monica, this is such a relief to see it, in writing, with references all over the place, that the safety factor is something men in my age-group shouldn’t have any fears about. Thanks, again, for spelling it out for us!
Kent, I am very glad to hear that!
I will soon publish some articles outlining the latest cardiovascular and prostate safety data with TRT…stay tuned… 🙂
I am glad to hear that this treatment is beneficial. It appears that since it is beneficial in man that it should transfer beneficially to women in menapause. women need the help and the benefit of such a treatment. women who do not have many choices this is one that would be helpful. I certainly hipe that the medical community is considering the treatment of women in this hormone replacement.
I agree with you that the importance of testosterone for women needs more attention that it is getting. I will be writing much more on that as well in the near future. 🙂
Fabulous post…Multiple beneficial effects of testosterone replacement therapy are very useful and knowledgeable information. Testosterone is a serious issue for men. Testosterone is an essential hormone produced by both men and women. Thank you for sharing this.