Considering how many people are on thyroid meds and or SSRI’s, it’s surprising – especially in the case of thyroid medications – how much confusion exists in the medical community on how best to treat people with hypothyroid.
I find many people feel they are often in some sort of battle between themselves and their doctor as to what doses, types, etc of thyroid meds they need. Frankly, I find most medical professionals do a sub par job of managing hypothyroid patients, and there’s simply no justifiable reasons for it any more.
A book called “Thyroid Disorders” written by a Dr Gilbert Daniels, listed as Co- Director of the Thyroid Clinic at Mass General Hospital makes for a good reference guide. The book was published in 2006, so I am assuming he’s still there. The book is written for physicians, specifically for GPs/family physicians vs. specialists. Most of the information would be basic rehash for the people here that have already done a lot of research on the topic, and most of what he recommends is in line with the standard recommendations. Some of Dr. Daniels comments below on T4/T3 combination therapy was supported by recent studies that found people on a combo therapy much prefer it over a T4 mono therapy. Since his book, there’s been study after study that supports T4/T3 combination therapy vs T4 mono therapy for those who either subjectively fail to thrive on T4 mono therapy, and or, those who do not adequately convert T4 to the active T3, yet very few doctors (at least in the United States) are aware of it, and once made aware, often refuse to even try it with their patients who continue to feel poorly on T4 alone. If you are one of those people, you need to have a conversation with who ever manages your thyroid condition, and if they refuse to work with you, find one who will. That’s how strongly I feel about the issue as someone who has personally had to deal with medical doctors over the years refusing to acknowledge the above.
Why the resistance is unclear, but one of them is they’re often under the impression that the inclusion of T3 will lead to risks of atrial fibrillation, increased blood pressure, thyrotoxicosis, cardiovascular complications, and arrhythmias. Yet, studies and clinical experience of those rare doctors willing to use T4/T3 combination therapy, simply don’t see it. As always, the dose makes the poison and proper dosing and management is the key success. For some, simply increasing the dose of T4 mono therapy was beneficial to patients. The real problem is, many medical doctors treat their thyroid patients via labs alone, vs labs plus subjective symptoms, and that’s a mistake, a mistake far too many suffer with years or decades without relief. It’s time that stopped!
Dr Daniels makes a few salient points regarding optimizing therapy, which seems to be the major issue for most people and clearly differs between individuals. A one size fits all approach to thyroid management does not work and is all too common among doctors sadly, and their patients suffer for it. Unlike many ‘traditional’ docs out there, Dr Daniels seems fairly open minded. For those looking for a decent reference guide to tests, diagnoses, etc, it’s a good little book.
It could also be helpful for when making your case that you are not happy with your current meds/dose, etc and the doc you are working with is resistant. For example, he states:
“Although thyroid function can be precisely, monitored, not all ‘optimally treated’ patients feel well. For example in one study in which patients were treated with increments of thyroid hormone, those whose T4 dose was increased by 25-50 mcg/d, resulting in a suppressed serum TSH, felt consistently better than those receiving the highest dose at which TSH could be maintained within the normal range. In another community population-based study, patients taking T4 felt psychologically less well than a matched control population.”
Possible explanations for the above findings he lists as:
o Some of these patients may have been subtly under treated. When hypothyroid patients remain symptomatic, the T4 dose should be increased until TSH reaches the lower normal range.
(Note, however, he’s clear to point out that an intact hyopthalamo-pituitary axis is necessary for TSH to reflect thyroid status appropriately and other measures such as free hormones and symptoms should be used in that situation in addition to TSH)
o The patients may have remained symptomatic because their symptoms were related to other disorders possibly associated with Hashimoto’s thyroiditis, such as depression.
o True physiological replacement of thyroid hormone may require both T4 and T3.
o Clinical deterioration after starting T4 therapy should raise the question of concomitant adrenal insufficiency, known as Schmidt’s syndrome.
For a ‘traditional’ endocrinologist I thought his comments above showed an open minded approach I wish more docs followed.
Finally, an excellent review paper recently published – Optimal Hormone Replacement Therapy in Hypothyroidism – A Model Predictive Control Approach – covers the topic in depth and also makes the case T4/T3 combination therapy often yielding the best results.
For Those on Selective Serotonin Reuptake I nhibitors (SSRI’s)
Additionally, and changing topics a bit here, but germane to the situation of many people, recent studies find that t3 augments the effects of SSRIs, even with treatment resistant major depressive disorder (MDD), so those on SSRIs not experiencing improvements may want to talk with their physician/therapist about adding a small amount of t3.
Recent t3 and SSRI studies of interest follow for those who enjoy reading study abstracts. Obviously, optimal thyroid levels are essential for weight management and general health. However, a well planned and science based nutrition and exercise program are just as important, if not more so, but some experience weight gain on SSRI’s and fail to respond well to those drugs. The addition of T3 may be of benefit in both cases:
Studies of interest:
1: J Clin Psychiatry. 2005 Aug;66(8):1038-42.
An open study of triiodothyronine augmentation of selective serotonin reuptake inhibitors in treatment-resistant major depressive disorder.
Depression Clinical and Research Program, Massachusetts General Hospital, Harvard Medical School, Boston 02114, USA.
OBJECTIVE: In an open trial, we investigated the efficacy of triiodothyronine (T(3)) adjuvant to selective serotonin reuptake inhibitors (SSRIs) in subjects with major depressive disorder (MDD) resistant to SSRI treatment. METHOD: Twenty subjects who met DSM-IV criteria for MDD (mean +/- SD age = 44.3 +/- 10.3 years; 55% [N = 11] women) and had failed to respond to a course of treatment of at least 8 weeks with an SSRI antidepressant were enrolled in a 4-week open-label augmentation treatment with T(3) 50 microg/day. Atypical and melancholic sub-types of MDD were diagnosed using Structured Clinical Interview for DSM-IV Axis I Disorders criteria. We administered the 17-item Hamilton Rating Scale for Depression (HAM-D-17) 4 times during the study (which was conducted between 2001 and 2003). RESULTS: During T(3) augmentation, the severity of depression decreased from an initial mean +/- SD HAM-D-17 score of 20.5 +/- 3.6 to a final HAM-D-17 score of 14.0 +/- 7.1 (p < .001). Seven subjects (35.0%) were treatment responders (HAM-D-17 reduction >or= 50%), and 6 subjects (30.0%) achieved clinical remission (final HAM-D-17 < .01) greater clinical improvement (final HAM-D-17 scores 6.6 +/- 1.8 vs. 16.4 +/- 4.5), and higher rates of treatment response (100% [5/5] vs. 13.3% [2/15]) and remission (80.0% [4/5] vs. 13.3% [2/15]), compared to subjects with nonatypical MDD. The 8 subjects with melancholic MDD experienced significantly (p < .05) greater depression severity at the end of the study compared to nonmelancholic MDD subjects (final HAM-D-17 scores = 18.3 +/- 6.6 vs. 11.1 +/- 6.1). CONCLUSION: Triiodothyronine augmentation of SSRIs may be a promising treatment strategy in SSRI-resistant MDD, particularly in subjects with the atypical MDD subtype.
_____________________
: J Affect Disord. 2006 Apr;91(2-3):211-5. Epub 2006 Feb 17.
T3 augmentation of SSRI resistant depression.
Department of Psychiatry, University of Toronto, ON, Canada.
PURPOSE OF STUDY: To investigate whether the addition of triiodothyronine (T3) helps relieve depressive symptoms in non-hypothyroid major depressive disorder patients who failed to respond to an adequate course of standard SSRI antidepressant treatments. METHODS: Patients who fulfilled the DSM-IV criteria for non-psychotic major depression, able to give informed consent, and failed to show satisfactory antidepressant response after a minimum of six weeks adequate treatment were recruited. To enter the study their Hamilton Depression (17-item HAMD) score had to be 18 or more, thyroid-stimulating hormone (TSH) value within the normal range, and a normal thyrotropin releasing hormone-stimulation test (TRH-ST). All patients continued taking the same SSRI which they had been taking before they entered the study. At the completion of TRH-SH they were all started on 25 microg of T3 and the dose was increased to 50 microg within a week when tolerated; they continued the combination of T3 and the SSRI for a minimum of three weeks. RESULTS: Twelve patients, comprising eight females and four males, entered the study. One female patient withdrew during the first week of side effects, eleven patients completed the trial. The patients ranged from 26 to 77 years of age, with the mean age for males and females being 52.3 and 45.1 years, respectively. Five patients were taking sertraline (mean dose = 130 mg/day) and 4 were taking citalopram (mean dose = 50 mg/day), two were on fluvoxamine (150 mg/day) and one patient was on 40 mg of paroxetine. The women took a mean daily dose of 40.6 microg of T3 for a mean duration of 3.75 weeks, while the men were on a mean daily dose of 43.8 mug of T3 for 3.5 weeks. T3 augmentation was associated with a statistically significant drop (p < .003) in the mean HAMD at end of the three weeks compared to baseline scores. Five patients (42%) showed >or=50% improvement on HAMD scores, with three achieving full remission (HAMD scores
___________________________
J Clin Psychiatry. 2001 Mar;62(3):169-73.
Triiodothyronine augmentation of selective serotonin reuptake inhibitors in posttraumatic stress disorder.
Department of Psychiatry, Hadassah-Hebrew University Medical Center,
BACKGROUND: There is considerable comorbidity of major depression and posttraumatic stress disorder (PTSD), and antidepressants have been reported to be effective in treating PTSD. Addition of triiodothyronine (T3) to ongoing antidepressant treatment is considered an effective augmentation strategy in refractory depression. We report the effect of T3 augmentation of antidepressants in patients with PTSD. METHOD: T3 (25 microg/day) was added to treatment with a selective serotonin reuptake inhibitor (SSRI) (paroxetine or fluoxetine, 20 mg/day for at least 4 weeks and 40 mg/day for a further 4 weeks) of 5 patients who fulfilled DSM-IV criteria for PTSD but not for major depressive disorder (although all patients had significant depressive symptoms). The Clinician-Administered PTSD Scale, the 21-item Hamilton Rating Scale for Depression, and the Clinical Global Impressions-Severity of Illness scale were administered every 2 weeks, and self-assessments were performed with a 100 mm visual analog mood scale. RESULTS: In 4 of the 5 patients, partial clinical improvement was observed with SSRI treatment at a daily dose of 20 mg with little further improvement when the dose was raised to 40 mg/day. This improvement was substantially enhanced by the addition of T3. Improvement was most striking on the Hamilton Rating Scale for Depression. CONCLUSION: T3 augmentation of SSRI treatment may be of therapeutic benefit in patients with PTSD, particularly those with depressive symptoms. Larger samples and controlled studies are needed in order to confirm this observation.
____________________
Am J Psychiatry. 2006 Sep;163(9):1519-30;
Comment in:
Am J Psychiatry. 2006 Sep;163(9):1484-6.
A comparison of lithium and T(3) augmentation following two failed medication treatments for depression: a STAR*D report.
Massachusetts General Hospital, 50 Staniford St., Boston, MA 02114, USA.
OBJECTIVE: More than 40% of patients with major depressive disorder do not achieve remission even after two optimally delivered trials of antidepressant medications. This study compared the effectiveness of lithium versus triiodothyronine (T(3)) augmentation as a third-step treatment for patients with major depressive disorder. METHOD: A total of 142 adult outpatients with nonpsychotic major depressive disorder who had not achieved remission or who were intolerant to an initial prospective treatment with citalopram and a second switch or augmentation trial were randomly assigned to augmentation with lithium (up to 900 mg/day; N=69) or with T(3) (up to 50 mug/day; N=73) for up to 14 weeks. The primary outcome measure was whether participants achieved remission, which was defined as a score < or =7 on the 17-item Hamilton Depression Rating Scale. RESULTS: After a mean of 9.6 weeks (SD=5.2) of treatment, remission rates were 15.9% with lithium augmentation and 24.7% with T(3) augmentation, although the difference between treatments was not statistically significant. Lithium was more frequently associated with side effects (p=0.045), and more participants in the lithium group left treatment because of side effects (23.2% versus 9.6%; p=0.027). CONCLUSIONS: Remission rates with lithium and T(3) augmentation for participants who experienced unsatisfactory results with two prior medication treatments were modest and did not differ significantly. The lower side effect burden and ease of use of T(3) augmentation suggest that it has slight advantages over lithium augmentation for depressed patients who have experienced several failed medication trials.
Will Brink is the owner of the Brinkzone Blog. Will has over 30 years experience as a respected author, columnist and consultant, to the supplement, fitness, bodybuilding, and weight loss industry and has been extensively published. Will graduated from Harvard University with a concentration in the natural sciences, and is a consultant to major supplement, dairy, and pharmaceutical companies.
His often ground breaking articles can be found in publications such as Lets Live, Muscle Media 2000, MuscleMag International, The Life Extension Magazine, Muscle n Fitness, Inside Karate, Exercise For Men Only, Body International, Power, Oxygen, Penthouse, Women’s World and The Townsend Letter For Doctors.
He’s also been published in peer reviewed journals.
Will is the author of the popular e-books, both accompanied by private members forum access , Bodybuilding Revealed & Fat Loss Revealed.
You can also buy Will’s other books on Amazon, Apple iBook, and Barnes and Noble.




Hi Will,
Like most hormonal issues, mainstream physicians are ill equipped educationally to handle deficiencies.
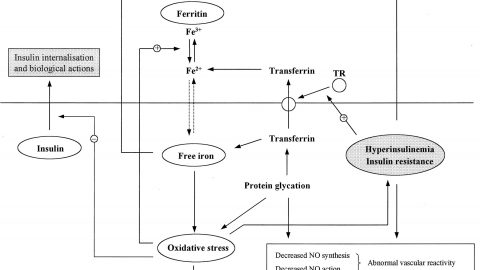
When prescribing thyroid, cortisol should always be monitored closely as it has a profound effect on T4/T3 metabolism. A patient with a mild cortisol deficiency will have elevated conversion of T4 to T3. This can result in an exacerbation of hypothyroidism or short term elevated T3 with effects of hyperthyroidism. The latter tends to mislead the physician into underdosing.
For most climates there is a winter and summer dose. If you are on thyroid meds and there are extremes in temperature between and summer and winter and your thyroid does remains constant, then your dose isn’t optimized.
Desiccated thyroid (T4/T3) meds tend to work much better. Namely Armour. Levothyroxine is the poorest choice.
Never allow your doc to treat your lab form. Lab data is for confirming a diagnosis and catching overt deficiencies and excesses. The dose should be adjusted based on clinical findings and history. As I have said many times, the lab’s ref range is just the 95% confidence interval for the lab’s reference group. Since this group is not in optimal health and the correct dose for you is not based on a statistical range, an experienced physician will know that you can be in the ref range and still have poor quality life.
Agreed Jim, why hormones in general seem to be so difficult to treat by the vast majority of docs (when most of the info is right under their nose) is unclear. I honestly think there’s almost an emotional/psychological aspect to it at this point where medical professionals (being human beings after all) have some sort of inherent bias toward hormones in general, clouding their judgement. I think it a worthy research paper for a psychologist. Look at the resistance to TRT. In the face of stacks of data, still viewed by so many as dangerous and or not warranted when both subjective symptoms and blood work say otherwise. Most disappointing to me has been discussions with endocrinologists who are supposed to have an advanced knowledge of the topic, yet so rarely do.
I would normally be in my own way and lacking alertness and energy. But I take a iodine/iodide combo at 12 mg (yeah, its high but it works) per day and I take tyrosine with it. But the tyrosine I have to vary according to feelings of enough alertness or too much and some anxiety. At times I might need 600 mg or so, and other times I skip it altogether. I probably average at least 100-200 mg per day. Caffeine caps work great when I have enough Iodine/tyrosine and not so great when I don’t have enough.
I have hypothyroidism and only brand name Synthroid works for me. I tried Armour. My T3 was through the roof, T4 was minimal and I was a zombie. For years I took Levoxyl. A few months prior to its recall, I was horribly sick as if I had suddenly developed Crohn’s disease. Taking Synthroid immediately reversed those symptoms, but I never fully recovered from whatever changes they did to Levoxyl but refused to admit they did. Recently I had my DNA analyzed, and I have several SNP’s that imply I may have problems processing several B and B related vitamins properly, especially B12, B6 and folate. Changing to hydroxy B12 drastically changed my overall health, but it has taken months to get there. I just started incorporating methyl B12 and methyl folate as I could not tolerate them eight months ago. I believe being on Aygestin for heavy bleeding increased my need for B vitamins and put me in a critical situation after being on it for 10 months. I don’t know how to describe the feeling other than my brain felt bad, like parts of my brain on either side of the corpus callosum were not getting enough nutrients or blood flow. I had a similar kind of feeling while on the “bad” Levoxyl. Try having any doctor take that description seriously! As bad as that situation was, Aygestin also affected my TSH levels. Finding the issue with processing B vitamins was the “fix” I could never get from any kind of thyroid medicine and my brain feels much better.