If you’re following the health news, you know that vitamin D currently is in the media spotlight, and rightly so. Will Brink just did a great podcast “Vitamin D3 – scam or panacea?“, giving an overview on the importance vitamin D. In this article I will expand upon some key points taken up in the podcast, and back up the case with a solid reference list of recent studies on the topic. I will also present some revealing prevalence stats on vitamin D insufficiency, in order to convince you to get your blood levels checked to find out your vitamin D status.
Vitamin D is interesting for several reasons:
1. The role of vitamin D for health promotion has undergone a paradigm shift.
While traditionally thought to only be important for development and maintenance of strong bones, an impressive body of scientific research has accumulated over the past decade, showing that adequate vitamin D levels are necessary to prevent many diseases, especially cardiovascular disease, high blood pressure, endothelial dysfunction, diabetes (both type-1 and type-2), the metabolic syndrome, chronic inflammation, cancer, osteoporosis (including falls and fractures), muscle weakness, cognitive dysfunction and mental illness, autoimmune diseases (e.g. multiple sclerosis, rheumatoid arthritis), infectious diseases, as well as infertility and adverse pregnancy and birth outcomes [1-24].
Vitamin D deficiency/insufficiency is associated with all-cause mortality [1], and supplementation has been shown to decrease mortality rates [25, 26]. It has been estimated that doubling vitamin D levels in the general population (from 21 ng/mL to 44 ng/mL) would reduce vitamin D-related disease mortality rate by 20%, and increase life expectancy with about 2 years [27].
2. Insufficient levels of vitamin D also have direct implications for fitness enthusiasts and athletic performance, due to the importance of vitamin D for muscle function (I will cover this in much more dept in an upcoming article) [28-39].
3. In contrast to other vitamins, vitamin D deficiency/insufficiency is very common (more on that below).
4. The vitamin D requirement for health promotion and protection against the mentioned diseases and muscle dysfunction is much higher than the dietary recommendations (RDA) for bone health [4, 40-45].
Having heard about all the vitamin D benefits you might wonder what is the optimal vitamin D level? How low is too low and how high is too high? How much vitamin D does one have to consume to reap all the benefits?
Let’s find out…
What are the blood level thresholds indicating vitamin D insufficiency?
The form of vitamin D that is measured in blood and used to indicate vitamin D status is called 25-hydroxy-vitamin D (abbreviated 25[OH]D) [9, 46]. So when I talk about blood vitamin D levels in this article, it is 25-hydroxy-vitamin D I am referring to (it’s easier for most people to think in terms of vitamin D levels than 25[OH]D or 25-hydroxy-vitamin D).
There is no official consensus about what is the optimal vitamin D level, and it is possible that different endpoints require different optimal vitamin D levels. However, based on the currently available data, prominent vitamin D researchers and authorities have presented the following guidelines:
Vitamin D status thresholds as defined by blood 25-hydroxy-vitamin D (25[OH]D) levels.
| ng/mL | nmol/L | Vitamin D status | Reference |
| below 20 20-30 over 30 50-60 over 150 |
50 50-75 75 125-150 375 |
Deficient Insufficient Sufficient Ideal level Risk for toxicity |
[47-49] [47-49] [18, 22, 41, 47, 48, 50-58] [4, 9, 22, 28] [9, 46, 59] |
Notes:
* Severe deficiency that causes softening of the bones occurs with levels below 10 ng/mL (25 nmol/L) [60].
* Blood (serum) levels of 25(OH)D are reported in either nanograms per milliliter (ng/mL) and nanomoles per liter (nmol/L).
* 1 ng/mL = 2.5 nmol/L
Traditionally, government issued health guidelines have stated that vitamin D levels of 20 ng/mL are sufficient. However, in light of new data prominent vitamin D researchers now recommend vitamin D levels in the range of 50-60 ng/ml, for both health promotion and athletic/physical performance [4, 9, 28]. As indicated in the table, even though this new recommended level is 2-3 times the old recommendation, it is far below the risk for intoxication and is thus a safe target to aim for in order to achieve all the vitamin D related health benefits (which is will cover in dept in upcoming articles).
How common is vitamin D insufficiency?
Low vitamin D status, i.e. vitamin D deficiency or insufficiency, is far more common than previously thought.
When looking at stats, it’s important to distinguish vitamin D deficiency from insufficiency. While severe vitamin D deficiency isn’t as prevalent, vitamin D insufficiency is:
* 36% of the US population is deficient, with vitamin D levels below 20 ng/ml [61].
* In a study on subjects characteristic of the US white population, it was found that only 18% have a vitamin D level over 30 ng/ml [62]. Thus, a whopping 82% are insufficient in vitamin D!
Similar results were found in the 2004 National Health and Nutrition Examination Survey (NHANES) [63] and in other analyses [58].
* To make things worse, data from (NHANES) showed that the number of persons with a vitamin D level below 30 ng/mL nearly doubled between the 1994 and 2004 [63].
Bearing in mind that the desired range as recommended by vitamin D research experts, is 50-60 ng/ml, these stats are alarming and underscore the fact that vitamin D insufficiency exists in epidemic proportions in the US. This vitamin D insufficiency epidemic spans across the globe [61].
How should I get my vitamin D?
The sources of vitamin D are sunlight exposure, food and supplements [9]. However, only a few foods are naturally rich in vitamin D [9]:
| Salmon, fresh wild caughtSalmon, fresh farmedSalmon, cannedSardines, canned Mackerel, canned Tuna, canned Egg yolk Fortified milk | 600–1,000 IU/3.5 oz vitamin D3100–250 IU/3.5 oz vitamin D3300–600 IU/3.5 oz vitamin D3300 IU/3.5 oz vitamin D3 250 IU/3.5 oz vitamin D3 236 IU/3.5 oz vitamin D3 20 IU/yolk vitamin D3 or D2100 IU/8 oz, usually vitamin D3 |
Thus, unless you eat oily fish every day (which would carry risk for toxicity from environmental contaminants), you cannot rely on your diet to cover your vitamin D needs.
Another source, the safety of which is controversial, is sunlight exposure. This is why vitamin D is called the “sunshine vitamin”. Because vitamin D can be produced by the skin upon sun exposure, it is actually not a vitamin in the traditional sense (per definition, vitamins are essential because they cannot be produced by the body). In fact, vitamin D is a pre-hormone to the hormone calcitriol (which is the active hormonal from of vitamin D that exerts effects on different tissues in the body). However, as said above, it is the vitamin D metabolite 25-hydroxy-vitamin D (25[OH]D) that is used to indicate vitamin D status and to guide supplementation needs.
Even though sun exposure theoretically is an effective vitamin D source, it cannot safely be relied on. A recent study showed that vitamin D supplementation is actually more effective than advised sunlight exposure for treating vitamin D deficiency [64]. The inferiority of sunlight exposure to improve and keep optimal vitamin D status is supported by findings of prevalent vitamin D insufficiency even in sunny Florida [65]. This was also underlined in a study of tanned prototypic “surfer dudes” (mean age 24 years) who overall reported an average of 22.4 hours per week of unprotected sun exposure [66]. Despite this abundant sunshine exposure, the mean blood vitamin D level was only 31 ng/mL (79 nmol/L), and 51% had a level below the recommended ideal 30 ng/mL (75 nmol/L) cutoff for sufficiency [66].
Also, the capacity to produce vitamin D in the skin is lower in dark skinned people, and diminishes as we get older [67, 68]. The darker skin types (III–VI) and the oldest people (>59 yr) are at the highest risk for not making enough vitamin D3 during the year from everyday outdoor exposures, even with a 2–3 week summer vacation [68]. People living in northern latitudes are especially at risk of not getting enough vitamin D producing UVB radiation from the sun [68, 69].
Another issue with sun bathing is the consequence of skin aging and risk of skin cancer. Unfortunately, the UVB radiation that produces vitamin D in the skin, is also the culprit causing skin cancer and wrinkling [70, 71]. This is a legitimate reason to not attempt to cover your vitamin D requirements by sun exposure. And even if sun exposure was a safe and reliable way to cover vitamin D needs, in today’s society with hectic work schedules most people don’t have much time to be out in the sun. It has been established that most adult Americans do not go outside enough to meet their minimum vitamin D3 needs all year [68].
Vitamin D supplements come as either vitamin D2 (ergocalciferol) or vitamin D3 (cholecalciferol) [4, 72] and in over-the-counter dosages of up to 10,000 IU. In the past there was a scientific “D-bate” over the efficiency of D2 vs. D3. However, a recent systematic review and meta-analysis of all studies published to date concluded that vitamin D3 is more effective at raising blood levels of vitamin D (i.e. 25-hydroxy-vitamin D) [73]. More specifically, vitamin D3 is approximately 87% more potent in raising and maintaining 25-hydroxy-vitamin D levels, and produces 2- to 3-fold greater body storage of vitamin D than does vitamin D2 [74]. Given its greater potency and lower cost, the vitamin D3 form should be the preferred supplement choice to elevate and maintain health promoting vitamin D levels.
Bottom Line
Now you know the importance of finding out your vitamin D level. Either ask your doctor to check it, or order a vitamin D blood test online without a doctor’s prescription if you don’t have health insurance. Life Extension offer great blood testing services, including vitamin D testing. Get your 25-Hydroxy-vitamin D Blood Test now!
If your blood level of 25-hydroxy-vitamin D shows that you are insufficient in vitamin D (which most folks are), you will need to get a vitamin D3 supplement to reap all the health and performance benefits from this multi-functional pre-hormone. Vitamin D supplementation is the fail-proof way to go in order to safely and effectively get your vitamin D level to the optimal 50-60 ng/mL range. Adequate vitamin D supplementation and sensible sunlight exposure to reach optimal vitamin D status are among the front line factors of prophylaxis for a spectrum of commons diseases.
In the next article I will explain that there is no clear cut vitamin D dose-response relationship because of the considerable variation in how individuals respond to vitamin D supplementation. The response to treatment varies with baseline vitamin D levels, body fatness, differences in activities of vitamin D metabolizing enzymes, skin pigmentation (race), season and geographic location (latitude). This is why it is so important that you check your baseline level and also keep monitoring it regularly, e.g. every 6 months, to see how you respond to vitamin D3 supplementation. In the next article I will cover supplemental vitamin D “loading” and maintenance dosages to raise your level fast and keep it there. I will also present studies that have reported mega-dosages of vitamin D intake, to give you a perspective, and cover safety and toxicological aspects. Stay tuned!
References:
1. Pludowski, P., et al., Vitamin D effects on musculoskeletal health, immunity, autoimmunity, cardiovascular disease, cancer, fertility, pregnancy, dementia and mortality-A review of recent evidence. Autoimmun Rev, 2013.
2. Rosen, C.J., et al., The nonskeletal effects of vitamin D: an Endocrine Society scientific statement. Endocr Rev, 2012. 33(3): p. 456-92.
3. Zhang, R. and D.P. Naughton, Vitamin D in health and disease: current perspectives. Nutr J, 2010. 9: p. 65.
4. Wacker, M. and M.F. Holick, Vitamin D – effects on skeletal and extraskeletal health and the need for supplementation. Nutrients, 2013. 5(1): p. 111-48.
5. Milaneschi, Y., et al., The association between low vitamin D and depressive disorders. Mol Psychiatry, 2013.
6. Mezza, T., et al., Vitamin D deficiency: a new risk factor for type 2 diabetes? Ann Nutr Metab, 2012. 61(4): p. 337-48.
7. Mitri, J., M.D. Muraru, and A.G. Pittas, Vitamin D and type 2 diabetes: a systematic review. Eur J Clin Nutr, 2011. 65(9): p. 1005-15.
8. Vuolo, L., et al., Vitamin D and cancer. Front Endocrinol (Lausanne), 2012. 3: p. 58.
9. Holick, M.F., Vitamin D deficiency. N Engl J Med, 2007. 357(3): p. 266-81.
10. Bosomworth, N.J., Mitigating epidemic vitamin D deficiency: the agony of evidence. Can Fam Physician, 2011. 57(1): p. 16-20, e1-6.
11. Zittermann, A., Vitamin D in preventive medicine: are we ignoring the evidence? Br J Nutr, 2003. 89(5): p. 552-72.
12. Wang, C., Role of vitamin d in cardiometabolic diseases. J Diabetes Res, 2013. 2013: p. 243934.
13. Baz-Hecht, M. and A.B. Goldfine, The impact of vitamin D deficiency on diabetes and cardiovascular risk. Curr Opin Endocrinol Diabetes Obes, 2010. 17(2): p. 113-9.
14. Chagas, C.E., et al., Focus on vitamin D, inflammation and type 2 diabetes. Nutrients, 2012. 4(1): p. 52-67.
15. Rosenblum, J.L., et al., Calcium and vitamin D supplementation is associated with decreased abdominal visceral adipose tissue in overweight and obese adults. Am J Clin Nutr, 2012. 95(1): p. 101-8.
16. Martini, L.A. and R.J. Wood, Vitamin D status and the metabolic syndrome. Nutr Rev, 2006. 64(11): p. 479-86.
17. Bikle, D., Nonclassic actions of vitamin D. J Clin Endocrinol Metab, 2009. 94(1): p. 26-34.
18. Cavalier, E., et al., Vitamin D and type 2 diabetes mellitus: where do we stand? Diabetes Metab, 2011. 37(4): p. 265-72.
19. Muscogiuri, G., et al., Can vitamin D deficiency cause diabetes and cardiovascular diseases? Present evidence and future perspectives. Nutr Metab Cardiovasc Dis, 2012. 22(2): p. 81-7.
20. Oosterwerff, M.M., et al., Serum 25-hydroxyvitamin D levels and the metabolic syndrome in older persons: a population-based study. Clin Endocrinol (Oxf), 2011. 75(5): p. 608-13.
21. Nagpal, J., J.N. Pande, and A. Bhartia, A double-blind, randomized, placebo-controlled trial of the short-term effect of vitamin D3 supplementation on insulin sensitivity in apparently healthy, middle-aged, centrally obese men. Diabet Med, 2009. 26(1): p. 19-27.
22. von Hurst, P.R., W. Stonehouse, and J. Coad, Vitamin D supplementation reduces insulin resistance in South Asian women living in New Zealand who are insulin resistant and vitamin D deficient – a randomised, placebo-controlled trial. Br J Nutr, 2010. 103(4): p. 549-55.
23. Nazarian, S., et al., Vitamin D3 supplementation improves insulin sensitivity in subjects with impaired fasting glucose. Transl Res, 2011. 158(5): p. 276-81.
24. Mitri, J., et al., Effects of vitamin D and calcium supplementation on pancreatic beta cell function, insulin sensitivity, and glycemia in adults at high risk of diabetes: the Calcium and Vitamin D for Diabetes Mellitus (CaDDM) randomized controlled trial. Am J Clin Nutr, 2011. 94(2): p. 486-94.
25. Bjelakovic, G., et al., Vitamin D supplementation for prevention of mortality in adults. Cochrane Database Syst Rev, 2011(7): p. CD007470.
26. Autier, P. and S. Gandini, Vitamin D supplementation and total mortality: a meta-analysis of randomized controlled trials. Arch Intern Med, 2007. 167(16): p. 1730-7.
27. Grant, W.B., An estimate of the global reduction in mortality rates through doubling vitamin D levels. Eur J Clin Nutr, 2011. 65(9): p. 1016-26.
28. Cannell, J.J., et al., Athletic performance and vitamin D. Med Sci Sports Exerc, 2009. 41(5): p. 1102-10.
29. Hamilton, B., Vitamin d and athletic performance: the potential role of muscle. Asian J Sports Med, 2011. 2(4): p. 211-9.
30. Ceglia, L. and S.S. Harris, Vitamin d and its role in skeletal muscle. Calcif Tissue Int, 2013. 92(2): p. 151-62.
31. Ceglia, L., Vitamin D and skeletal muscle tissue and function. Mol Aspects Med, 2008. 29(6): p. 407-14.
32. Pfeifer, M., B. Begerow, and H.W. Minne, Vitamin D and muscle function. Osteoporos Int, 2002. 13(3): p. 187-94.
33. Boland, R.L., VDR activation of intracellular signaling pathways in skeletal muscle. Mol Cell Endocrinol, 2011. 347(1-2): p. 11-6.
34. Girgis, C.M., et al., The roles of vitamin D in skeletal muscle: form, function, and metabolism. Endocr Rev, 2013. 34(1): p. 33-83.
35. Birge, S.J. and J.G. Haddad, 25-hydroxycholecalciferol stimulation of muscle metabolism. J Clin Invest, 1975. 56(5): p. 1100-7.
36. Hamilton, B., Vitamin D and human skeletal muscle. Scand J Med Sci Sports, 2010. 20(2): p. 182-90.
37. Hazell, T.J., J.R. DeGuire, and H.A. Weiler, Vitamin D: an overview of its role in skeletal muscle physiology in children and adolescents. Nutr Rev, 2012. 70(9): p. 520-33.
38. Wassner, S.J., et al., Vitamin D Deficiency, hypocalcemia, and increased skeletal muscle degradation in rats. J Clin Invest, 1983. 72(1): p. 102-12.
39. Daly, R.M., Independent and combined effects of exercise and vitamin D on muscle morphology, function and falls in the elderly. Nutrients, 2010. 2(9): p. 1005-17.
40. Cashman, K.D., et al., Estimation of the dietary requirement for vitamin D in healthy adults. Am J Clin Nutr, 2008. 88(6): p. 1535-42.
41. Bischoff-Ferrari, H.A., et al., Estimation of optimal serum concentrations of 25-hydroxyvitamin D for multiple health outcomes. Am J Clin Nutr, 2006. 84(1): p. 18-28.
42. Aloia, J.F., et al., Vitamin D intake to attain a desired serum 25-hydroxyvitamin D concentration. Am J Clin Nutr, 2008. 87(6): p. 1952-8.
43. Vieth, R., et al., Randomized comparison of the effects of the vitamin D3 adequate intake versus 100 mcg (4000 IU) per day on biochemical responses and the wellbeing of patients. Nutr J, 2004. 3: p. 8.
44. Vieth, R., P.C. Chan, and G.D. MacFarlane, Efficacy and safety of vitamin D3 intake exceeding the lowest observed adverse effect level. Am J Clin Nutr, 2001. 73(2): p. 288-94.
45. Vieth, R., Experimentally observed vitamin D requirements are higher than extrapolated ones. Am J Clin Nutr, 2009. 90(4): p. 1114-5; author reply 1115-6.
46. Holick, M.F., et al., Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab, 2011. 96(7): p. 1911-30.
47. Holick, M.F., Vitamin D: a D-Lightful health perspective. Nutr Rev, 2008. 66(10 Suppl 2): p. S182-94.
48. Holick, M.F., Vitamin D status: measurement, interpretation, and clinical application. Ann Epidemiol, 2009. 19(2): p. 73-8.
49. Hollis, B.W., Circulating 25-hydroxyvitamin D levels indicative of vitamin D sufficiency: implications for establishing a new effective dietary intake recommendation for vitamin D. J Nutr, 2005. 135(2): p. 317-22.
50. Vieth, R., et al., The urgent need to recommend an intake of vitamin D that is effective. Am J Clin Nutr, 2007. 85(3): p. 649-50.
51. Heaney, R.P., The case for improving vitamin D status. J Steroid Biochem Mol Biol, 2007. 103(3-5): p. 635-41.
52. Vieth, R., Why the minimum desirable serum 25-hydroxyvitamin D level should be 75 nmol/L (30 ng/ml). Best Pract Res Clin Endocrinol Metab, 2011. 25(4): p. 681-91.
53. Mason, R.S., V.B. Sequeira, and C. Gordon-Thomson, Vitamin D: the light side of sunshine. Eur J Clin Nutr, 2011. 65(9): p. 986-93.
54. Souberbielle, J.C., et al., Vitamin D and musculoskeletal health, cardiovascular disease, autoimmunity and cancer: Recommendations for clinical practice. Autoimmun Rev, 2010. 9(11): p. 709-15.
55. Bischoff-Ferrari, H.A., et al., Benefit-risk assessment of vitamin D supplementation. Osteoporos Int, 2010. 21(7): p. 1121-32.
56. Hanley, D.A., et al., Vitamin D in adult health and disease: a review and guideline statement from Osteoporosis Canada. CMAJ, 2010. 182(12): p. E610-8.
57. Bischoff-Ferrari, H.A., The 25-hydroxyvitamin D threshold for better health. J Steroid Biochem Mol Biol, 2007. 103(3-5): p. 614-9.
58. Binkley, N., R. Ramamurthy, and D. Krueger, Low vitamin D status: definition, prevalence, consequences, and correction. Endocrinol Metab Clin North Am, 2010. 39(2): p. 287-301, table of contents.
59. Holick, M.F. and T.C. Chen, Vitamin D deficiency: a worldwide problem with health consequences. Am J Clin Nutr, 2008. 87(4): p. 1080S-6S.
60. Bikle, D.D., Vitamin D: newly discovered actions require reconsideration of physiologic requirements. Trends Endocrinol Metab, 2010. 21(6): p. 375-84.
61. Holick, M.F., et al., Guidelines for preventing and treating vitamin D deficiency and insufficiency revisited. J Clin Endocrinol Metab, 2012. 97(4): p. 1153-8.
62. Marantes, I., et al., Is vitamin D a determinant of muscle mass and strength? J Bone Miner Res, 2011. 26(12): p. 2860-71.
63. Ginde, A.A., M.C. Liu, and C.A. Camargo, Jr., Demographic differences and trends of vitamin D insufficiency in the US population, 1988-2004. Arch Intern Med, 2009. 169(6): p. 626-32.
64. Wicherts, I.S., et al., Sunlight exposure or vitamin D supplementation for vitamin D-deficient non-western immigrants: a randomized clinical trial. Osteoporos Int, 2011. 22(3): p. 873-82.
65. Levis, S., et al., Vitamin d deficiency and seasonal variation in an adult South Florida population. J Clin Endocrinol Metab, 2005. 90(3): p. 1557-62.
66. Binkley, N., et al., Low vitamin D status despite abundant sun exposure. J Clin Endocrinol Metab, 2007. 92(6): p. 2130-5.
67. The Australian and New Zealand Bone and Mineral Society, et al., Risks and benefits of sun exposure: Position Statement, 2007.
68. Godar, D.E., et al., Solar UV doses of adult Americans and vitamin D(3) production. Dermatoendocrinol, 2011. 3(4): p. 243-50.
69. Kimlin, M.G., Geographic location and vitamin D synthesis. Mol Aspects Med, 2008. 29(6): p. 453-61.
70. Wolpowitz, D. and B.A. Gilchrest, The vitamin D questions: how much do you need and how should you get it? J Am Acad Dermatol, 2006. 54(2): p. 301-17.
71. El Ghissassi, F., et al., A review of human carcinogens–part D: radiation. Lancet Oncol, 2009. 10(8): p. 751-2.
72. Thacher, T.D. and B.L. Clarke, Vitamin D insufficiency. Mayo Clin Proc, 2011. 86(1): p. 50-60.
73. Tripkovic, L., et al., Comparison of vitamin D2 and vitamin D3 supplementation in raising serum 25-hydroxyvitamin D status: a systematic review and meta-analysis. Am J Clin Nutr, 2012. 95(6): p. 1357-64.
74. Heaney, R.P., et al., Vitamin D(3) is more potent than vitamin D(2) in humans. J Clin Endocrinol Metab, 2011. 96(3): p. E447-52.


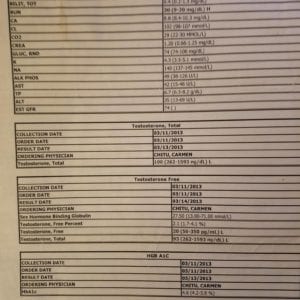




I recently had a few blood tests done (Testosterone, Cholesterol, CRP, etc, inspired by the “it’s in your blood” article), and everything was normal or even quite favorable, however my Vitamin D came out at a shockingly low 6.6 ng/ml!! I guess I’m a prime example of how widespread this deficiency is, even in otherwise healthy people.
Better start popping them pills!
Indeed you are!
Being so severely vitamin D deficient i’d recommend you very large dosing dose. Is you doctor willing to prescribe you vitamin D treatment? If not, I’d recommend 50,000 IU per day for 10 days, and then 12,000 IU per day for 20 days. After that, get your vitamin D level checked and adjust the dose based on your new reading.
I will cover the issue of vitamin D dose-response and strategies to treat vitamin D deficiency in my next article. Let us know how you respond and how treatment of your vitamin D deficiency makes you feel. Being so deficient I can tell you are going to notice a major strength improvement in the gym. Keep us posted 🙂
Thanks for your answer! FYI, I am from Austria, and living in Germany right now. Doctors here aren’t exactly forward-thinking (most in the US probably aren’t either, but at least there are good resources (LEF eg) to find the good ones.). Most doctors, even though they are MD’s, also offer quackery treatments (homeopathy is really big here). I have a doctor, who I go to the get prescription allergy medicine (which is OTC in the US), but that’s about it (I actually saw a brochure in the waiting room once about how angels help us heal). If I went to my doctor and asked her about Vitamin D treatment, she wouldn’t know what I was talking about.
Anyway, I actually just went to a lab on my own and got these tests done – no doctor involved. I am now taking 7,000 IU’s (2,000 from the LEF mix plus I added 5,000). I guess I am a little reluctant to go to these high doses on my own, even though risk of toxicity is probably non-existent at my levels. I think I am going to put in some effort into finding a better doc (there’s got to be some).
I am curious, since you mentioned a strength improvement. Something I have always had, is feeling extremely drained and fatigued the day after a hard gym session. I can do a lot of work, push myself hard etc, but it definitely affects me the next day. Could this also be related to the deficiency?
If your doctor isn’t informed about the seriousness of vitamin D deficiency, get another one!
Then I’d suggest you start with a loading period of 3 x 7000 IU per day for 4 weeks, then go down to 7000 IU per day for 6 weeks, and after that do another blood test.
Maybe. But you will probably notice more during your workouts as your vitamin D levels start increasing.
Great article and very useful for many people (like many of other articles made by your and Will as well).
By reading the article I found myself a little bit puzzled at the part:
…”Vitamin D supplements come as either vitamin D2 (cholecalciferol) or vitamin D3 (ergocalciferol)”…
I’m using D3 supplementation for last two years and it really made me wondering if I might read it wrong or it was just a typo mistake while you were typing the article. I’m using D3 (cholecalciferol) and when I checked about D2 it showed up as ergocalciferol, so I guess you can quickly correct that typo unless I’m dealing with wrong information and wrong impression and I would be more then grateful if you confirm it so I can update my “knowledge base” in my head 🙂
p.s. can’t wait to see your next article about dosages so I can compare with the ones I’m using (until I get my blood test done to check the exact value).
That was a typo, my bad. I just corrected it, should be:
vitamin D2 (ergocalciferol)
vitamin D3 (cholecalciferol)
You said “A recent study showed that vitamin D supplementation is actually more effective than advised sunlight exposure for treating vitamin D deficiency”
Considering that foods are relative low in Vitamin D and that millions of years of evolution has our bodies producing vitamin D from sun exposure, should be an indicator where we should be getting our Vit.D. Hard to believe that mother nature loses out to synthetic vitamin D.
Just a thought,
Always enjoyed your articles.
Keep them coming.
Vitamin D deficiency was probably rare among our ancestors. The fact that it is on the rise means it is our modern lifestyle that is to blame.
I have also thought about this and am curious why these deficiencies occur, even in the “surfer dudes”. Two things I could think of (just what I think could be a possibility, I don’t have data to verify it), is that food 100,000 years ago was probably more nutritious than today, and people literally spent the whole day outside, not just 22.4 hours per week. It wasn’t always in the sun of course, but it could still have been enough to make a difference.
Monica, great article! You should really look into vitamin k2 to go with your follow up article. You should not take high doses of d3 without k2. I have been conducting a high dose d3 experiment on myself for the last 40 days because my levels were low. I am trying to bring my level to 60. I am taking 1 LEF super k for every 10,000 iu’s of d3 as recommended. I believe vitamin k will be the next big thing. It’s worth you looking into! Thanks, Lisa
Yes, there’s an interesting synergy between vitamin K2 and Vitamin D, and calcium metabolism. And like you say, K2 is (like vitamin D) the subject of intense research, that deserves an article in its on right.
I’d say it is more deleterious to supplement with calcium without K2, than vitamin D without K2. Of course, getting them all together is the best approach.
Monica,
How does the ng/mL translate into the i.u.’s listed on the vitamin label?
Great artilcle by the way, as usual.
thanks,
Jeff
As I will explain in my upcoming article; there is no clear-cut dose-response relationship between vitamin D intake and blood levels. The same dose can elevate blood vitamin D levels [ie 25(OH)D] to different degrees in different people. This is why it is so important to monitor your levels. But I will provide some guidelines.
Great article, look forward to reading the next instalment.
You’re welcome 🙂
Will and Monica, Great info as usual. As a 59 yr. old guy I had my Vitamin D level checked 6 months ago and it was 19 (ref. range 33-100). My doc told me to take 1000 units of Vitamin D3 once a day. Last week I had a regular Dr. visit and had routine blood work done again. So after 6 months of taking 1000 units of Vitamin D once a day, my level was still only 21. My Dr. then said take 1000 units of Vitamin D3 twice a day. He neglected to say when to take them. I have read all your Vitamin D3 should be taken in the morning, with your largest meal but not at night because it can cause sleep disturbances.
I know you are not doctors…but he is not a nutritionist. So can you suggest a typical dosage and the proper time(s) that people ordinarily take Vitamin D3 and get the best results so I can intelligently discuss it with him? Thanks!
Thanks for sharing your experience. I will go into much more dept on dose-response in the follow-up article, but here is what I’d recommend somebody with a baseline of around 20 ng/mL:
Start with a loading dose of vitamin D3: 28-30,000 IU/day for 15 days, then go down to 7-8,000 IU/day for 20 days. After that, get your vitamin D level checked again and adjust the dose based on your new reading.
Vitamin can be taken anytime, but is best absorbed with fat rich meals. It’s highly unlikely that it will cause sleep disturbances. Being fat soluble, the dose can be taken either all at once (severe deficiencies are actually treated by injections of 50,000-100,000 IU, so you don’t have to worry about taking high doses at one time), or split up over the day. I though personally prefer to split the dose up over the day.
Monica, Thanks for your prompt and thorough reply. Gee, 30,000units a day for 2 weeks SOUNDS high. Is there any danger of Vitamin D3 toxicity or overdose?
Vitamin D has an extremely large safety margin;
30,000 IU/day x 15 days = 450,000 IU in 15 days
Deficiencies are safely and successfully treated with single loading mega-doses in the range of
600,000 IU:
Effect of a single oral dose of 600,000 IU of cholecalciferol on serum calciotropic hormones in young subjects with vitamin D deficiency: a prospective intervention study.
Cipriani C, et al; J Clin Endocrinol Metab. 2010 Oct;95(10):4771-7
Once you’ve got your level up to 50-60 ng/mL, a maintenance dose of 5,000-10,000 will keep you there. I will go into more dept on this in my follow up article.
Ok, Thanks Monica.
Did you listen to the radio show linked in the Monica’s article above? There’s plenty of additional info there. Follow her dosing advice. As you experienced the “high” doses you took, did very little for your levels. I take 5000IU per day, in addition what what I get in a multi and my food and some sun, and that gets me right in the 50-60 range.
When it comes to vitamin D dosing, one has to distinguish loading dose (to elevate one’s vitamin D level) and maintenance dose (to keep the elevated level).
Thank you so verymuch for writing this email.
What I was wondering though, was the fact, that you used
measures, nt familiar to most persons onthe street.
Please, would you explain the different measures used
using micrograms, not those. millimoles or IUs, which are
usually used by doctors and other people, who try to mix
our thoughts to not see thetruth. It is very common to
use milli- and micrograms, when speaking about vitamins
in general, isn’t it? I had to look for those other measures
from Wikipedia to understand anything, but it really would
be more useful to common people to understand, to use
one type of measures only.
Thank you very much for your very beneficial articles,
dear Monica.
1 microgram vitamin D = 40 IU vitamin D
10 microgram vitamin D = 400 IU vitamin D
100 microgram vitamin D = 4000 IU vitamin D
200 microgram vitamin D = 8000 IU vitamin D
There you go.
One type of measure would indeed be nice, but of course does not exist, even between scientists or doctors at times and across cultures (meters, ft, inches, gallons, ounces, etc, etc), so we still have to make those conversions to make sense of it from our own reference points.
Thank you Monica for such an in depth and interesting article. I love your work and look forward to reading everything you write. I am in awe of your outstanding knowledge and so appreciate you passing it on. Look forward to the coming follow ups on this topic and and any others you write. Thank you and have a great day.
Thanks Cindy; I’m glad you appreciate my work.
So, was the follow-up ever published? If so, where?
This article states that getting sunlight on the skin may not be a reliable way to obtain adequate blood levels of Vitamin D, as indicated by a study done using tanned surfer dudes in Florida, who had less than optimal blood levels of Vitamin D, even though they got a lot of sunlight on their skin.
One explanation for those surprisingly low blood levels of Vitamin D is this: according to Dr. Nicholas Perricone, in order to obtain adequate nloodevels of Vitamin D from sunlight, you cannot shower, bathe or go swimming within 8 hours of sunbathing. Dr. Perricone says that if you do those, it washes the Vitamin D from your skin, before the Vitamin D can penetrate the skin, and get into the blood. Plus, Dr. Perricone says that you cannot shower, bathe or swim before sunbathing either; because doing those washes tge oils from your skin, that are needed for the production of Vitamin D in the skin.
And Dr. Joseph Mercola says that you have to wait at least 48 hours after sunbathing, before you take a shower, a bath or go swimming.
So that might explain why the Vitamin D blood levels in those test subjects were so low, kn spite of all of their sunlight exposure on the skin.
I’d have to see some data that due to bathing too fast, that prevented them from obtaining the benefits, but it does not pass the smell tests for me. It’s as likely, or more so, their mag status is part of that equation. Finally, Sun converts D2 -> D3, and the rest is up to the body (liver and kidneys) and we know some can take very high doses of D3 and get very little response, so that again, suggests something else is going on, like mag deficiency per my most recent article.
I’m assuming everyone takes some sort of multivitamin. Are the levels of Vitamin D in a typical multivitamin not sufficient?
Depends on the multi and what 25OHD levels are achieved. Article outlines best ways to approach that, which starts by getting your levels checked to assess what your next moves are there.
I take 5,000 IU’s a day with magnesium. My blood panel says my D is at 57.7 which is right in the middle of toxicity and too low. I guess I’m good. Here’s hoping our AlphaJoe comes soon.
Should ship any day now!